This advertorial is sponsored by Philips.
The benefits of utilizing intravascular ultrasound (IVUS) in peripheral vascular interventions has been widely demonstrated in the literature. In nearly every vascular bed studied, we have seen an improvement in overall outcomes. Over the last several years, clinical data in support of IVUS has exploded, including the first-ever randomized controlled trial (RCT) of the modality that demonstrated its use has changed treatment plans in 79% of arterial cases.1
In addition, an analysis of over 500,000 patients demonstrated that IVUS improved outcomes with a 27% reduction in major adverse limb events (MALEs).2 The use of IVUS in the venous vasculature has also demonstrated clinically significant improvements in outcomes. A real-world analysis of IVUS use in the treatment of venous disease demonstrated a 28% risk reduction for repeat intervention, hospitalization or death.3
These data build on the VIDIO (Venogram vs. IVUS for diagnosing iliac vein obstruction) study findings, which like the arterial RCT, demonstrated IVUS changed treatment plans in nearly 60% of venous cases,4 identifying patients with severely symptomatic central pelvic vein occlusive disease that would have been missed with other routine imaging. With these compelling data in mind, a group of 40 cross-specialty physicians published a consensus paper regarding the use of IVUS in peripheral interventions, where they agreed that the use of IVUS was strongly recommended in all interventional phases of both arterial and venous procedures.5
With advanced visualization tools like IVUS, we can get a 360-degree view inside the vessel, allowing us to accurately assess the severity of disease and create a specialized approach to treatment.
Case review: Arterial example
Here, we present a case of a patient with severe ischemic rest pain and an ankle-brachial index (ABI) of 0. The patient was a prior smoker who had multiple prior interventions for critical limb ischemia (CLI) and tissue loss. In 2021, the patient had a second femoral-to-tibial artery bypass and was lost to follow-up.
On angiogram, there was redemonstration of superficial femoral artery and popliteal artery stent occlusion, and chronic occlusion of both the anterior tibial and posterior tibial target bypasses. There was no arterial reconstitution of viable open or endovascular target vessels in the foot.
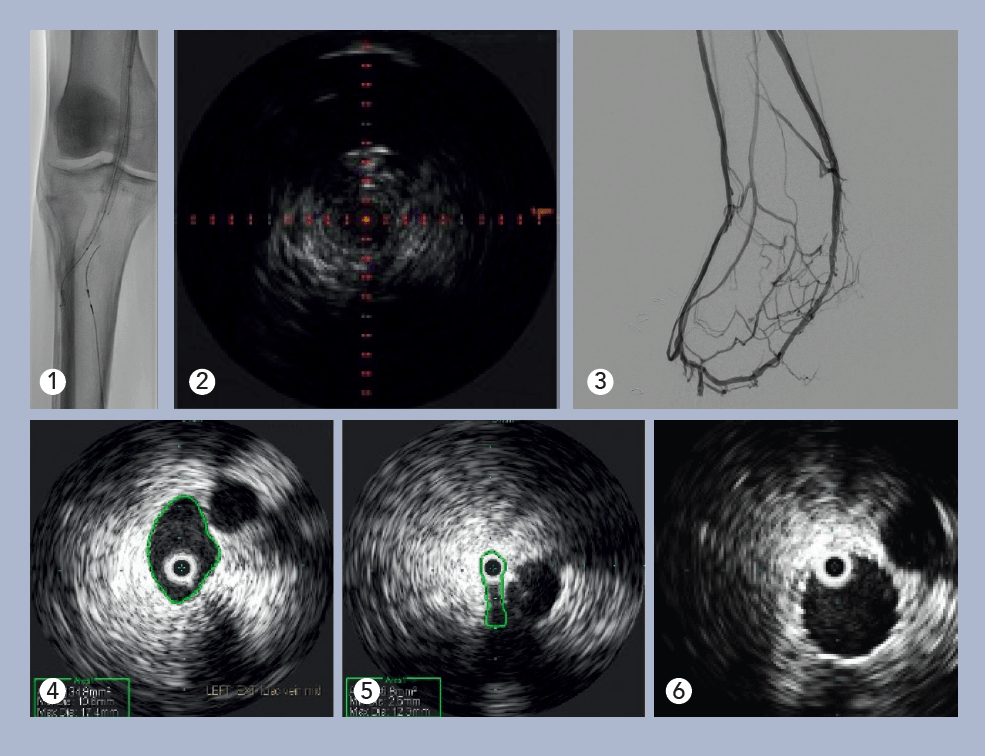
Deep venous arterialization (DVA) was performed using the Pioneer Plus catheter for IVUS-guided arterial re-entry (see Figure 1). Visualization of the popliteal artery re-entry target by IVUS allowed for rapid crossing from the posterior tibial venous access site (see Figure 2).
The use of covered self-expanding stents and percutaneous balloon angio-and venoplasty formalized the iatrogenic arteriovenous fistula. Post-intervention IVUS using the Reconnaissance .018 OTW IVUS catheter verified appropriate luminal gain and aided identification of incomplete venous valvular disruption in the foot (see Figure 3). Target areas of venous outflow were addressed with repeated venoplasty. At one-month follow-up, the patient reported marked symptomatic improvement, and non-invasive duplex imaging showed DVA patency.
Venous example
 Here, we present a case of a 65-year-old Caucasian female with a three-year history of left leg swelling, heaviness and achiness, which improved with elevation.
Here, we present a case of a 65-year-old Caucasian female with a three-year history of left leg swelling, heaviness and achiness, which improved with elevation.
She had no history of prior deep vein thrombosis (DVT), venous interventions, peripheral artery occlusive disease, leg trauma, congestive heart failure or chronic kidney injury. The symptoms improved overnight while in bed, and returned the next day. She woke up in the morning free of these symptoms, but, by evening, she was quite uncomfortable. On physical exam, she had erythema in the gaiter distribution of the lower- and mid-calf circumferentially, with skin induration and edema of the calf. She had no open wounds. She had no visible varicose veins.
On left lower-extremity venous duplex ultrasound exam, the patient had no significant infrainguinal superficial vein disease. There was significant multi-segmental deep vein reflux, with a reflux time of >1 second. There was no acute DVT, nor any evidence of deep vein scar to indicate a prior DVT.
Evaluation of the central veins in the pelvis with venogram revealed no focal iliac vein stenosis or filling defect, and there were no cross-pelvic or lumbar collaterals noted. IVUS with the Visions .035 system was performed, identifying a severe cranial external iliac vein (EIV) stenosis (73%), compared to the normal suprainguinal caudal EIV, due to a non-thrombotic iliac vein lesion (NIVL). Normal suprainguinal caudal EIV and severe cranial external iliac vein stenosis (see Figures 4 and 5).
Post-angioplasty and stent, there was no residual stenosis (Figure 6). On follow-up exam one week later, the stent was widely patent on duplex ultrasound, and the patient remarked, “I can see my ankle again!”
The heaviness, achiness and erythema resolved during the following weeks. Through five years of follow-up, she had no recurrence of her symptoms or physical findings of chronic venous hypertension and insufficiency.
References
- Allan R, Puckridge P, Spark J, et al. The Impact of Intravascular Ultrasound on Femoropopliteal Artery Endovascular Interventions. J Am Coll Cardiol Intv. 2022 Mar, 15 (5) 536–546. https://doi.org/10.1016/j.jcin.2022.01.001
- Divakaran S, Parikh SA, Hawkins BM, et al. Temporal Trends, Practice Variation, and Associated Outcomes With IVUS Use During Peripheral Arterial Intervention. JACC Cardiovasc Interv. 2022;15(20):2080- 2090. doi:10.1016/j.jcin.2022.07.050
- Divakaran S, Meissner MH, Kohi MP, et al. Utilization of and Outcomes Associated with Intravascular Ultrasound during Deep Venous Stent Placement among Medicare Beneficiaries. J Vasc Interv Radiol. 2022;33(12):1476-1484.e2. doi:10.1016/j.jvir.2022.08.018
- Gagne PJ, Tahara RW, Fastabend CP, et al. Venography versus intravascular ultrasound for diagnosing and treating iliofemoral vein obstruction. J Vasc Surg Venous Lymphat Disord. 2017;5(5):678-687. doi:10.1016/j.jvsv.2017.04.007
- Secemsky EA, Mosarla RC, Rosenfield K, et al. Appropriate Use of Intravascular Ultrasound During Arterial and Venous Lower Extremity Interventions. JACC Cardiovasc Interv. 2022;15(15):1558-1568. doi:10.1016/j.jcin.2022.04.034
Steven D. Abramowitz, MD, is a vascular surgeon in Washington, D.C. Abramowitz has been compensated for his services for Philips’ further use and distribution. Paul J. Gagne, MD, is a vascular surgeon with the Vascular Care Group in Darien, Connecticut. Gagne has been compensated for his services for Philips’ further use and distribution.












