This advertorial is sponsored by Silk Road Medical.

For Scott Berman, MD, patient responses when confronted with an explanation of the extent of their asymptomatic carotid disease tend to be quite stark. They are either so petrified of having a stroke that they express clearly that they want to be operated on as a matter of urgency, the Tucson, Arizona-based vascular surgeon explains, or else they are steadfastly against surgery under any circumstances.
That’s why Berman sees patient-reported outcomes as a crucial component to factor into certain areas of his treatment decision-making. So, a recent patient satisfaction survey—which demonstrated those carotid disease patients who underwent transcarotid artery revascularization (TCAR) recovered more quickly than those who received carotid endarterectomy (CEA)—confirmed what already seemed intuitive.
“As soon as we started doing TCAR, we could see early on that these patients were recovering a lot more quickly than CEA patients,” says Berman, of Pima Heart & Vascular, a study author who contributed a tranche of patients to the survey. “The overall experience seemed to be better.”
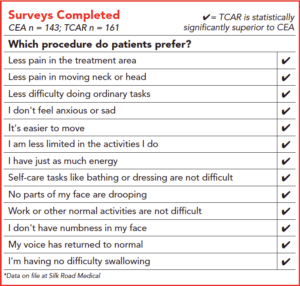
The survey, conducted across nine medical centers, drew 304 responses (161 TCAR; 143 CEA) from 64 patients across a total of 13 questions on post-procedure pain, lifestyle limitations and activity ability. A hospital staff member at each of the nine participating hospitals conducted the surveys over the phone once per week for four weeks.
Berman contributed 10 patients—five each for TCAR and CEA. “It really reinforced what we had observed—that TCAR patients seemed to have a less eventful recovery after revascularization than endarterectomy patients,” he says. “The overall experience has seemed to be better with TCAR, and the early results with this survey support that.”
Among the key findings, the study—which was completed Silk Road Medical—established that patients who were treated with TCAR experienced less pain over all time periods than those who underwent CEA. TCAR patients also reported significantly less facial numbness, swallowing issues, facial drooping and voice changes over time than their CEA counterparts. Furthermore, TCAR patients reported more ease in completing ordinary tasks 48 hours to one week post-procedure.
“Even in my subset, we were able to see that there was statistical significance in many areas, including pain control and returning to activities,” notes Stacey LeJeune, MD, of Surgical Associates and a community hospital vascular surgeon in Wausau, Wisconsin, another author involved in the patient satisfaction study.
LeJeune contributed 20 patients to the survey—10 for each procedure.
“As someone who does a lot of carotid surgery, both endarterectomy and TCAR are overall felt to be relatively safe. Patients tend to do well, and the majority go home the next day. But this study is very interesting because it gets the patients’ perspective on the little things that matter to them during their recovery. I was greatly surprised by the one-week post-procedure results regarding patients returning to driving their car.”
The relevant data from the survey show that 71.4% of TCAR patients reported having driven their car at the one-week post-procedure mark versus just 25% of CEA patients responding that they had done so.
Berman drills further into what the data mean for patients in their day-to-day lives in the days after treatment.
“Globally, patients seemed to recover quickly,” he reflects. “if you look at the actual numbers: less pain, less trouble moving, able to drive. Return of normal voice, lack of numbness, no facial droop. With all of these things, they really reinforced what we had already observed.”
Berman sees such patient-reported outcome measures as sitting at the vanguard of surgeons and interventionalists being better healthcare spending stewards.
“We have to make sure that the treatment we provide is actually helping the patient, and making them feel better,” he says.
“There are some things that are a little objective—if a patient has a giant aneurysm, we don’t operate on them to make them feel better; we operate on them to prevent death. Claudication is the classic example of when we try to improve a patient’s lifestyle, so we certainly should be able to measure whether or not lifestyle improved as a result of our treatment.”
Carotid disease sits somewhere in between the aortic aneurysm and claudication analogy, Berman explains. “We certainly want to improve or reduce the risk of stroke, but that risk of stroke impacts how people conduct their life.”
LeJeune, meanwhile, looks at patient satisfaction through the lens of appropriate patient selection.
“Through my experience performing TCAR on my own patients, and also teaching the procedure to many colleagues, it’s clear to see how much faster, smoother and less invasive this procedure is, particularly for those who have the right anatomy,” she explains.
“Patient selection is key to good outcomes, and I think that we are going to continue to see positive outcomes for these patients—both standard risk and high risk— as we move forward. As a surgeon my priority is a good clinical outcome, but if we’ve proven that that is equivalent, it then gets down to time, cost and patient satisfaction. In a world where patient satisfaction is very important for a lot of reimbursement type of issues, I think patient-reported outcomes are very important.”
Berman points toward the future direction of the survey and how it had dovetailed with his experience investigating patient-reported outcomes in the claudication arena.
“With claudication, there are a lot of validated surveys of patient-reported outcomes,” he observes. “There are none for carotid disease.” Berman says the challenge now is to take “a robust questionnaire” and put it through the rigors of statistical validation.
“Vascular surgeons in general are very data driven, and quick to challenge data to make sure it’s been collected appropriately,” he adds. “That’s the next step but this is an important first step.”
Which is only going to become more important in light of recent events regarding Centers for Medicare & Medicaid Services (CMS) moves to incorporate patient preference: “I think it’s important to have this kind of data from patients to make informed decisions,” says Berman.
For LeJeune, bolstering patient enrollment is key to strengthening the survey data going forward. As the authors look at the survey as it currently stands, the results point to a truism, she adds.
“Having this good subset of patient responses is supporting what we know already, but as clinicians sometimes understimate—the part of a patient’s healing where we assume they are doing well. We see them back a few weeks later and don’t appreciate these nuances.
“This study has teased out some of that, showing how much faster TCAR patients feel better and recover in the short-term.”












