A preliminary report lends evidence to support female sex being considered as an independent risk factor for new stroke occurrence after carotid revascularization in symptomatic patients, according to a research team from Italy who presented at the International Chapter Forum during the 2022 Vascular Annual Meeting (VAM) in Boston (June 15–18).
A preliminary report lends evidence to support female sex being considered as an independent risk factor for new stroke occurrence after carotid revascularization in symptomatic patients, according to a research team from Italy who presented at the International Chapter Forum during the 2022 Vascular Annual Meeting (VAM) in Boston (June 15–18).
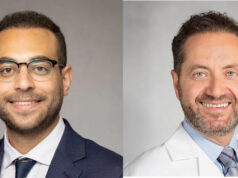
Presenting author Pasqualino Sirignano, MD, a vascular surgeon at the University of Rome in Rome, Italy, detailed how the team’s analysis was carried out amid uncertainty in the Italian guidelines over specific recommendations for female patients undergoing revascularization treatment for both symptomatic and asymptomatic carotid disease.
“We reviewed our experience to better review any possible gender-related difference [in outcomes] in patients treated in Italy for a symptomatic carotid lesion—either by carotid endarterectomy [CEA] or carotid artery stenting [CAS],” he told the forum.
The retrospective study matched CAS patients treated within one month of symptom onset—pulled from the IRONGUARD 2 study—with CEA patients collected by the University of Rome during the same period.
The researchers were aiming to evaluate any new stroke occurrence within the first 30 days of follow-up. They included 265 patients, 72 of whom were women. Half of the patient pool was treated in the urgent or emergent setting, Sirignano said. Five out of nine new strokes were recorded among female patients, he continued.
“The most important thing we found was that, even though there were only 72 women in the cohort, the nine strokes were recorded within this female population, and no differences were found at baseline between the two sexes,” Sirignano explained.
“Emergent patients treated within 24 hours of symptom onset have worse outcomes compared to patients treated in the urgent or elective setting. Looking at multivariate analysis, once again we found that female sex, and timing of surgery, were the only two independent risk factors for worse outcomes after both carotid endarterectomy and carotid artery stenting.”
Sirignano concluded: “Although this is another preliminary report on this rising topic, we have to admit that female sex should be considered as an independent risk factor for new stroke occurrence after carotid revascularization in symptomatic patients.”
Session moderator Palma Shaw, MD, noted how Sirignano and colleagues had mentioned timing of procedures impacted worse outcomes. “We have seen in prior presentations that intervening within 48 hours of an event has a worse outcome,” she said. “Are you changing your approach to intervention in [the] acute [setting]?”
He said that his practice had already been altered, explaining: “We try to treat patients between three and seven days from symptom onset whenever it’s possible. But for unstable patients, we really don’t know what to do—unstable meaning crescendo, transient ischemic attack, or recurrent stroke. These were treated during the first 48 hours, and that was the reason for worse outcomes.”
Shaw suggested the data produced was being obscured by the inclusion of such patients and that removing them might elucidate a difference.