A new analysis that shows current smokers who undergo carotid endarterectomy (CEA) for asymptomatic carotid stenosis are at increased risk of long-term stroke and death compared to former or never smokers helps reinforce the importance of physicians talking to patients about quitting their smoking habit.
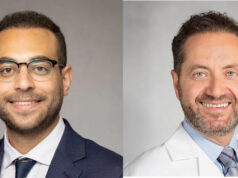
That was one of the key messages from the authors behind study findings showing a stroke rate among current smokers that was nearly twice as great as their former-smoker—defined as those who quit at least 30 days prior to surgery—and never-smoker counterparts. The data were reported at the 2024 Midwestern Vascular Surgical Society (MVSS) annual meeting in Chicago (Sept. 12–14). In an interview with Vascular Specialist, presenting author Hassan Chamseddine, MD, a research fellow at Henry Ford Health in Detroit, Michigan, describes the rationale behind digging into the Vascular Quality Initiative (VQI) in order to try to uncover evidence around the benefit from smoking cessation amid questions over CEA use among the patient population at hand.
“Currently, the Society for Vascular Surgery [SVS] recommends an endarterectomy for patients with an asymptomatic carotid stenosis if their stenosis is greater than 70%,” he explains.
“The evidence for the benefit of endarterectomy in this population comes from landmark trials—ACAS and ACST-1—but those trials are very old, and they are currently under increased scrutiny because the medical therapy arm back then does not reflect contemporary medical management. More recent studies—including the SPACE-2 trial—did not show any difference between CEA and best medical therapy in this population. And, all over the country, there is some doubt over the benefit, or necessity, of endarterectomy in asymptomatic patients.”
The research team—led by senior author Loay Kabbani, MD, vice chair of surgery for research and program director of the vascular surgery fellowship at the same institution—looked at all members of the patient population undergoing CEA from 2013–2023 logged in the VQI. Of the 77,664 included, 24% were current, 51% former and 25% never smokers.
The data showed the three groups had similar rates of perioperative complications, but, at 18-month follow-up, former smokers exhibited strokes comparable to never smokers—and both were “significantly lower” than current smokers (0.8%, 0.9% and 1.5%, respectively), Chamseddine points out.
In terms of major adverse cardiac events (MACE)—a combination of stroke, myocardial infarction and death—quitting smoking at least 30 days prior reduced MACE risk among former smokers when compared to current smokers, “but not by as much as those who never smoked,” adds Chamseddine.
Kabbani says the results help highlight a dual purpose. “Number one, this shows the benefit of smoking cessation for the patient, but [number two] also for the physician: If I’m a physician and I’m seeing a patient with asymptomatic disease that has significant stenosis, and there is a question mark about the benefit of the operation, if we want the patient to have the best long-term outcome, we really need to convince them to stop smoking before the operation. They do better in the long run in multiple settings, including decreased myocardial infarction and death.”
Kabbani underscores the importance of physician efforts around the subject of cessation: “Time and time again, we see that if a physician talks to a patient about quitting smoking, they have twice as much chance of stopping.”