Based on 30 years of experience, researchers have concluded that aneurysms of the superior mesenteric artery (SMA) are “relatively stable” and that those <20mm may be safely monitored with surveillance imaging. The experience also suggests that operative treatment should be considered if the aneurysms are symptomatic and that patients with vasculitis or fibromuscular dysplasia may need closer follow-up.
Presenting these findings at the Society for Vascular Surgery’s Vascular Annual Meeting (SVS VAM 2021), Grayson S. Pitcher, MD, an integrated vascular surgery resident at the Mayo Clinic in Rochester, Minnesota, notes that the study represents one of the largest series on aneurysms of the SMA and its branches.
“SMA aneurysms are rare and the SVS currently recommends repair of all SMA aneurysms and pseudoaneurysms regardless of size,” Pitcher stated. However, he stressed that the rupture rates of true aneurysms versus pseudoaneurysms vary significantly, with a much lower risk for true aneurysms.
The presenter detailed that two recent, small series suggest SMA aneurysms <20mm may be safe to observe. In light of this, Pitcher and colleagues at the Mayo Clinic aimed to review the centre’s 30-year experience with aneurysms of the SMA and its branches, determine their growth rate, and evaluate predictors of growth.
The research team conducted a retrospective review of all patients diagnosed with an aneurysm of the SMA or one of its branches—excluding pseudoaneurysms and mycotic aneurysms—in the period 1988–2018. Demographics, presentation, etiology, anatomic characteristics, and treatment modalities were taken into consideration. Endpoints included outcomes, growth, and predictors of growth.
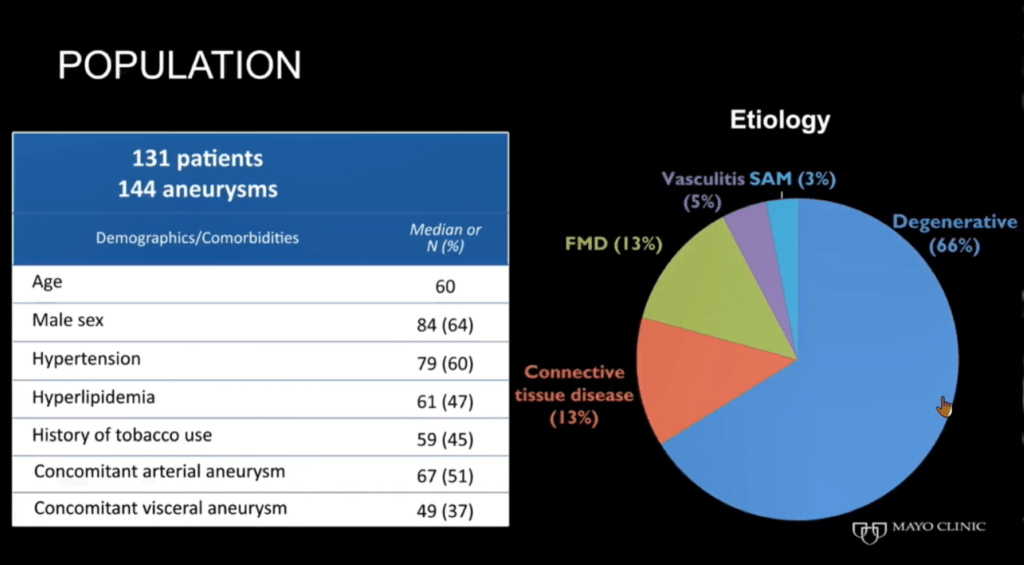
Pitcher communicated that a total of 131 patients, or 144 aneurysms, were included in the study. The average age of the patients was 60, 84 (64%) were male, and 66% of the aneurysms were degenerative, representing the most common etiology. The majority of the aneurysms were found incidentally, with only 27% being symptomatic.
Growth rate of the aneurysms was first estimated using linear regression. However, only 16% had a growth rate of ≥1mm per year. Due to the large number of aneurysms without any change in size, aneurysms were dichotomized by slope and a categorized analysis was performed using logistic regression.
Addressing the VAM audience, Pitcher reported: “Initial aneurysm size was significantly associated with growth rate for fusiform aneurysms only, meaning initial size is only predictive of growth for fusiform aneurysms.” The odds ratio (OR) for the fusiform aneurysm growth rate was 1.13 (95% confidence interval [CI], 1–1.3), with a p-value of 0.02. Initial aneurysm size was not significantly associated with saccular (OR, 0.91; 95% CI, 0.76–1.1; p=1.1) or dissection-associated aneurysms (OR, 1.2; 95% CI, 0.91–1.5; p=0.2).
The team then used logistic regression models to assess the effect of multiple variables on growth. Pitcher said that while the team evaluated a range of variables, the overwhelming majority were not associated with growth.
The presenter revealed that symptomatic status was significant and that acute abdominal pain (OR, 5.91; 95% CI, 1.56–22.41; p=0.0009) and chronic abdominal pain (OR, 3.76; 95% CI, 1.06–13.13; p=0.04) were significantly associated with growth rate.
Finally, Pitcher informed the audience that there were only two ruptures in the team’s series. One of these ruptures occurred in a 24mm saccular branch aneurysm and the other in a 12mm fusiform branch aneurysm. He added that only one of the ruptures occurred in an aneurysm less than 20mm in size out of a possible 106 possible aneurysms.