A study examining outcomes between different carotid revascularisation procedures has concluded that transcarotid artery revascularisation (TCAR) and carotid endarterectomy (CEA) both represent a “reasonable choice” in severe chronic kidney disease (CKD) and haemodialysis patients—but transfemoral carotid artery stenting (TF-CAS) appears more likely to result in worse outcomes.
“And, additionally, the majority of these patients are surviving long enough to benefit from the stroke risk reduction provided by surgery,” said Elisa Caron, research fellow in vascular surgery at Beth Israel Deaconess Medical Center in Boston, USA. At the 2024 Vascular Annual Meeting (VAM; 19–22 June, Chicago, USA), Caron reported an analysis of Vascular Quality Initiative (VQI) patients with estimated glomerular filtration rate (eGFR) <30ml/min/1.73m2, or on haemodialysis, undergoing TCAR, CEA or TF-CAS between 2016 and 2023.
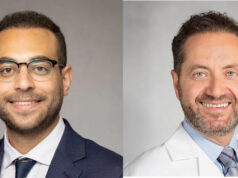
Presenting on behalf of her co-authors, including senior author Marc L Schermerhorn, chief of vascular and endovascular surgery at Beth Israel Deaconess Medical Center, Caron relayed data from 13,042 VQI patients with eGFR <30, 2,355 of whom were on haemodialysis.
The majority of outcomes—across both symptomatic and asymptomatic patients—were found to be “fairly similar” between TCAR and CEA, including stroke/death, with both procedures falling within SVS guidelines regarding perioperative stroke and death. However, CEA was linked with a trend towards slightly higher odds of stroke/death/myocardial infarction (MI), as per the analysis’ primary outcome, in addition to higher odds of MI when considered independently. Similar trends continued when the researchers looked specifically at the subgroup of haemodialysis-only patients, according to Caron.
Turning to findings on overall long-term survival, the presenter relayed that TCAR and CEA were once again similar, as survival rates were nearly 80% with both procedures across all asymptomatic patients and only dropped slightly to around 70% in the haemodialysis-only group at five years. She also noted that these trends endured among symptomatic patients, with rates dropping to around 70% across the full eGFR <30 and haemodialysis cohort.
In addition, regarding those who underwent TF-CAS, Caron reported that—prior to statistical weighting—these patients were more likely to be symptomatic, to present with stroke, and to undergo surgery in urgent/emergent settings, compared to TCAR and CEA patients. They also had more baseline comorbidities. But, “even after weighting for symptom status and comorbidities, TF-CAS still underperformed and did not meet SVS guidelines” she continued, with stroke, death and overall long-term survival being among the areas where TF-CAS produced inferior outcomes versus TCAR and CEA, across both asymptomatic and symptomatic patients.
Following Caron’s presentation, session moderator Chelsea Dorsey, MD, associate professor of surgery at UChicago Medicine in Illinois, commented that “these patients are incredibly fragile” and, as such, “the more granular information we have about how to approach them, the better”. Dorsey went on to ask the presenter how she feels these new data may impact people’s clinical practices moving forward.
“I think that patient selection will always play a big role,” Caron responded. “The VQI certainly gives us very granular data but, at the end of the day, it’s not the same as the patient sitting in front of you, and I think that will still have a big impact. That said, I think it’s at least reasonable to consider surgery in these patients—I know some people are hesitant to do so, so this at least provides evidence to support the decision of whether to intervene. But, again, patient selection is still going to be crucial.”