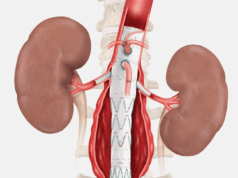
Thirty-day and one-year data from the STABLE II study have been published in the April 2020 issue of the Journal of Vascular Surgery (JVS) by Joseph V. Lombardi, MD, professor and chief of vascular surgery at Cooper University Hospital, Camden, New Jersey, and colleagues. The results demonstrate favorable clinical and anatomical outcomes for the treatment of rupture and malperfusion in the setting of acute, complicated type B aortic dissection (TBAD) with the Zenith dissection endovascular system from Cook Medical.
The authors note that the aim of the study was to evaluate the safety and effectiveness of the Zenith composite device design—covered stent graft and bare metal stent—for the treatment of patients with acute, complicated TBAD presenting with aortic rupture and/or vessel malperfusion.
In this prospective, nonrandomized, multicenter study, 73 patients (65.8% male; mean age, 60.7 years) with acute, complicated TBAD were enrolled between August 2012 and January 2015 to receive treatment with the Zenith dissection endovascular system in the U.S. and Japan.
Lombardi and colleagues detail that the primary safety endpoint was the rate of freedom from major adverse events at 30 days, and the primary effectiveness endpoint was the rate of survival at 30 days. The article published in JVS reports primary outcomes at 30 days and follow-up results through one year, reflecting study data as of March 2018.
Of 73 patients, 20 presented with aortic rupture (27%) and 57 presented with branch vessel obstruction/compromise (78%), including four patients presenting with both conditions. The covered stent graft was used in all patients (median, 1; range 1–3; one stent graft used in 64.4%; 47/73), and the bare metal dissection stent was used in 58 of 73 patients (79.5%).
As reported in JVS, thirty-day mortality occurred in five patients (6.8%): one procedure related, three unrelated to dissection repair and one indeterminate. Thirty-day major adverse events included myocardial infarction (1.4%), bowel ischemia (1.4%), renal insufficiency/renal failure requiring dialysis (6.8%), stroke (6.8%), paraplegia or paraparesis (5.5%), and prolonged ventilator support (13.7%).

Lombardi et al also state that nine deaths occurred from 31 to 365 days (only one death related to dissection repair) and the Kaplan-Meier estimate of freedom from all-cause mortality was 80.3±4.7% at one year.
Furthermore, within 365 days, nine of 73 patients (12.3%) underwent 10 secondary interventions and no patients required conversion to open surgery.
At the 12-month follow-up, complete or partial thrombosis of the false lumen was seen in 100% of patients (46/46) within the stent graft region and in 97.4% of patients (38/39) within the dissection stent region.
Finally, growth (>5mm) of the maximum transaortic diameter was observed in 14.9% of patients (7/47) in the stent graft region and in 38.5% of patients (15/39) within the dissection stent region at 12 months.
Lombardi and colleagues remark that the STABLE II data were originally presented at the 2016 Vascular Annual Meeting of the Society for Vascular Surgery (June 8–11) in National Harbor, Maryland. The Zenith device was approved by the Food and Drug Administration (FDA) in early 2019, with the first patient treated in the U.S. with the device in April the same year.
The authors note that five-year follow-up is ongoing.