 In response to recent articles in the lay press suggesting vascular surgeons were performing unnecessary procedures, Vascular Specialist medical editor, Malachi Sheahan, has asked me to write an editorial based on a talk I presented at the 2023 VEITHsymposium. At that meeting I provided data demonstrating which specialties are treating vascular patients and the rate of insurance denials dependent on provider specialty. I was originally reluctant. I had stopped writing editorials for Vascular Specialist because I had said all that I had on my mind. I was also concerned that, eventually, I would write a piece that readers would find so controversial that I would never be able to show my face in public again.
In response to recent articles in the lay press suggesting vascular surgeons were performing unnecessary procedures, Vascular Specialist medical editor, Malachi Sheahan, has asked me to write an editorial based on a talk I presented at the 2023 VEITHsymposium. At that meeting I provided data demonstrating which specialties are treating vascular patients and the rate of insurance denials dependent on provider specialty. I was originally reluctant. I had stopped writing editorials for Vascular Specialist because I had said all that I had on my mind. I was also concerned that, eventually, I would write a piece that readers would find so controversial that I would never be able to show my face in public again.
Well, here it is. I am going to come right out and say it in big, bold, black-and-white letters: “We need the insurance industry to save vascular patients and vascular surgeons.” To those few of you still reading, please stay with me. I am not suggesting that we continue the current system of prior authorization, since it is time-consuming, expensive, a nuisance for the provider and patient, and still does not guarantee quality care. Rather, I am going to propose a different system that I think has merit.
But first, here is some background as to how I came to the unfortunate conclusion that these companies could be the answer and not the problem. This will require that I detail some of the data that I addressed at the VEITHsymposium and my takeaway from the recent barrage of articles about unnecessary atherectomy. Further, how an American Board of Vascular and Endovascular Surgery (ABVES) aligns with my proposal, and why I keep urging that the Society for Vascular Surgery (SVS) change its name to the American College of Vascular and Endovascular Surgery (ACVES).
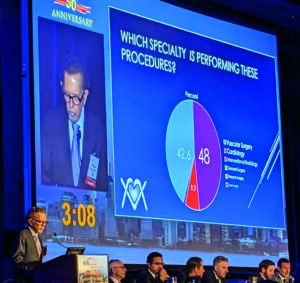
First, which specialty is responsible for most of vascular surgery in the United States? For the last two years I have been involved in developing and overseeing a major insurance carrier’s 100% outpatient Medicare Advantage prior authorization (PA) program involving 10 endovascular codes dealing with iliac, femoropopliteal and tibial arteries (Codes 37220–372230), and recently all vascular surgery. Medicare Advantage programs are now insuring more than 50% of all Medicare participants, so my experience has provided me a good overview of who is doing what and why. Cardiologists accounted for 48% of the requested PAs, with 42.6% from vascular surgeons, 8.3% from interventional radiologists, and 1% from general surgeons, thoracic surgeons, or nephrologists. There was a geographic variation with vascular surgeons, cardiologists, and interventional radiologists requesting, for example, 40%, 53%, and 6% PAs in Florida; 42.6%, 28.7%, and 28.7% in Texas; and 63%, 26%, and 11% in New York State, respectively. Irrespective of the variation, these data clearly show that, overall, vascular surgeons are probably doing less than half of the vascular procedures in the U.S. Now that the Centers for Medicare & Medicaid Services (CMS) has approved carotid stenting for asymptomatic patients, it is likely that cardiologists will take away even more procedures.
Diminishing voice
The fact that cardiology is now dominant has enormous repercussions. It diminishes the voice of vascular surgeons such that government entities, insurance companies, the lay press, and the public will turn to cardiologists and their societies for information, advice and treatment. This must have a negative impact on the viability of vascular surgeons’ practices and on patients’ health. Now, why do I say that it will affect patient health?
The answer to that also comes from my program, which has evaluated well over 20,000 requests for PA. Last year I presented a small sample of 1,488 PA requests (946 original PA, 172 peer-to-peer, and 370 appeals) for outpatient procedures from 20 states, with New York, Texas and Florida accounting for the majority. All PAs were evaluated predominantly by vascular surgeons or, on occasion, Board certified interventional cardiologists. Subsequent peer-to-peer discussions were performed by vascular surgeons. Let me assure you that this program was initiated because the company was convinced that abusive practices were causing harm not only to its bottom line, but also to its members’ (patients’) health and well-being. Since there is only one Local Carrier Determination (LCD 35998) dealing with non-cardiac stents, and since that LCD can only be used in six states for outpatient care, most insurance companies have developed their own documents outlining indications and appropriate use criteria. Some also use proprietary guidelines such as InterQual.1 For the most part, these are carefully researched, well-written attempts to curtail unnecessary procedures, yet ensure that necessary ones are authorized.
Our program predominantly used InterQual but also SVS appropriate use guidelines,2 as well as guidelines sponsored by the American College of Cardiology and American Heart Association.3 Overall denial rates were 44.8% for initial PAs, 45.8% for peer-to-peers, and 41% for appeals. Denials were more frequent for PA requests from cardiologists (56%) than interventional radiologists (47%) and vascular surgeons (30%). Admittedly, some denials were for lack of information or incorrect coding, but many were because patients were being rushed to the office-based lab (OBL) without attempts at conservative therapy. Some case scenarios attributed to cardiologists and interventional radiologists may shock even the most jaded reviewer. For example: a request to perform tibial atherectomy for claudication on a dialysis patient who one month previously had the peroneal artery perforated requiring two units of blood transfusion, fasciotomy, and resultant myocardial infarction; superficial femoral artery (SFA) and tibial atherectomy performed via pedal approach yet no prior or post attempt to treat proximal complete occlusion of the common iliac, external iliac and common femoral arteries; a patient with clearly defined significant femoropopliteal and tibial disease and a leg ulcer booked for an arteriogram but first having bilateral saphenous vein ablations thus destroying the potential for a tibial saphenous vein bypass; and now that we are reviewing all aspects of vascular surgery, an epidemic of PAs to treat “May-Thurner syndrome” affecting octogenarians with bilateral ankle swelling and congestive heart failure.
Since many of these latter requests are coming out of Florida, I suspect that May-Thurner syndrome must be caused by mosquito bites, as this would be the only way this epidemic could be explained. Further, radiologists are now offering endovascular embolization of genicular arteries to treat arthritis of the knee. In one case, the radiologist performed one of these procedures on a knee contralateral to a below-knee amputation and where the SFA was already showing evidence of atherosclerosis. What an amazing indictment that about half of all requests from these other specialists were denied.
Need I say more about how the expanded role of cardiologists will affect vascular patients? Well, if this is not sufficient, what about all the recent articles in the lay press? There is now an avalanche of material detailing the abusive use of atherectomy predominantly by cardiologists. However, as our PA program highlights, it is not just atherectomy but all the peripheral endovascular procedures.
‘Operate, Medicate and Dilate’
We must also recognize that, unfortunately, vascular surgeons accounted for 30% of the denials in this Medicare Advantage program. In a past editorial for Vascular Specialist, I made it abundantly clear that I believed that vascular surgeons, like the Knights of the Round Table (or more aptly, the rectangular table?) in the Arthurian legend, follow a chivalrous code of honor that guides us in placing a patient’s well-being ahead of financial reward. We ride out, catheter, stent and knife at the ready to defeat the malevolent atherosclerotic enemy. We proudly fly our banner proclaiming that only we “Operate, Medicate and Dilate.” We denounce other specialists involved in vascular care as Dark Knights whose evil intent is to plunder, their poor behavior induced by disparate payment schedules that favor dilating, rather than operating or medicating.
Yet, I am now chagrined to acknowledge that we too have knights who forsake their code of chivalry—vascular surgeons who value the attainment of wealth or prestige as their raison d’être. Perhaps a few examples of PAs requested by vascular surgeons will highlight that not all vascular surgeons follow appropriate guidelines: a stroke patient is wheelchair-bound and has no complaints relating to her legs but the duplex scan shows a “serious” SFA 80% occlusion that, if it occludes, can cause amputation; a request to treat an occluded anterior tibial artery at the same time as an SFA endovascular treatment for claudication, yet the posterior tibial and peroneal arteries are widely patent; an iliac angioplasty for claudication in a patient on home oxygen with limiting shortness of breath while being treated concomitantly for lung cancer; and four repetitive procedures within six months to treat recurrent right SFA occlusions with a patent popliteal and two-vessel runoff, yet no discussion of a surgical alternative? We need to make these “Dark Knights” aware of how their actions have a negative effect on the rest of us. Because, if left unchecked, castigation in the media and government action will punish all vascular surgeons and our legendary contributions to the management of vascular disease will fade from memory, just like Arthur and his knightly court.
Before I move on, let me speak to those of us who try to follow exemplary practice. Let us look deeply at our own experience and assess whether the following scenarios may be impacting what we do. In general, endovascular procedures are much easier to perform than open surgery, so a stent rather than a bypass. Complications may not be as devastating, so perhaps an inclination to intervene earlier in the disease process. As endovascular procedures replace open surgeries, new graduates and even older surgeons may begin to feel uncomfortable performing complex surgeries, so an angioplasty when a bypass may be preferable. Use a well-reimbursed new technology, though unproven, since it has a novel cache that can be advertised to referring physicians. Do some of these scenarios seem familiar?
Now let us return to the articles that were published in the New York Times and ProPublica since they are painting vascular surgeons with the same paint brush as cardiologists. It would take a highly educated layperson to realize that vascular surgeons accounted for very few of the 200 or so accused of overutilization since the word used most frequently is “vascular” not “cardiology,” and the authors often referred to the procedures as surgeries. So perhaps for the first time, the lay public is becoming aware of vascular surgeons, but surely this is not the way we had hoped? Let’s face it, the magician David Copperfield could not make vascular surgeons more invisible than we are now. Dr. Alan Dietzek, in his presidential address to the Society for Clinical Vascular Surgery,4 titled his first chapter, “The anonymity of our specialty,” and the following quotation remains true today. “Why are we still not recognized as the go-to physicians for the treatment of vascular disease? Why are we still fighting a battle for recognition that never seems to end? When will it change and how can we change it? Will our specialty survive?” Alan goes on to make an impassioned case for an American Board of Vascular Surgery (ABVS) independent from the American Board of Surgery (ABS), and he has remained committed to this quest.
I am suggesting that it rather be named the American Board of Vascular and Endovascular Surgery. Recently, cardiologists have approached the American Board of Medical Specialties (ABMS) requesting that their Board separate from the American Board of Internal Medicine, thus establishing a separate Board of Cardiovascular Medicine. If vascular surgery does not achieve its own board first, it will finally relegate vascular surgeons to being second-class purveyors of vascular treatment. Soon, I suspect the American College of Cardiology will adopt the name “American College of Cardiovascular Medicine.” That will be even more devastating; however, we cannot prevent it from happening. What we need instead is to immediately adopt a name change for the SVS. Some years ago, when the logo of the SVS was about to change, I suggested it was an opportune time to give up on the name Society for Vascular Surgery and rather become the American College of Vascular and Endovascular Surgery (ACVES). This has an imprimatur that will result in respect for its members and its messaging. It is more important now than ever before. Now, some will say it is too costly to change the name of the SVS and to have a separate ABVES. Stay tuned because my proposal will also pay for these changes. Together with the American Board of Vascular and Endovascular Surgery (ABVES), these renamed and new organizations will restore our preeminent position as the primary thought leaders and providers of vascular care.
To summarize, it is apparent that cardiology is taking over much of the management of vascular surgery patients in the U.S. The quality of their care is suspect. However, we must admit that some vascular surgeons do not offer optimal care either. Part of the reason for cardiologists’ increasing supremacy is that vascular surgeons have failed to market who they are and what they do. By allowing the ABS to represent vascular surgeons, we have abrogated our ability to stand as a unique entity. The SVS has not been aggressive in marketing vascular surgeons and even the name of the Society does not assure that vascular surgeons are the go-to specialists for vascular interventions. Insurance companies are aware of an increasing number of unnecessary procedures and are ramping up prior authorization programs. Hence my proposal.
Program of spot-checks
I propose that the American College of Vascular and Endovascular Surgery, in conjunction with the ABVES, develop the following program. Member vascular surgeons agree to have 10 procedures a year spot-checked randomly by the carrier after the procedures have been completed. In return, participating physicians will not require PAs for their patient procedures and surgeries. The review will include actual images rather than just reports since the written word can manipulate the truth, but images do not lie. If patients had wounds or varicose veins, photographs would also be provided. The review will be performed by Board-certified vascular surgeons who have been rigorously trained by a program developed by the ABVES. The reviewers will be required to be thoroughly versed in Medicare rules as they apply to vascular surgery, the various LCDs and their jurisdictions, and appropriate use guidelines and peer reviewed manuscripts selected by the ABVES. Before being accredited as a certified reviewer, they will have to undergo a test developed and run also by the ABVES. The program will also assist in procuring and paying for state licensure where necessary. Appropriate insurance will also be provided. Importantly, these reviewers will be well compensated for their work. All would have to sign an agreement that they will not review a potential competitor, or someone closely affiliated. A peer-to-peer will be mandatory before any denial. The goal should be remedial education and not punishment. Denials will be reviewed by a second reviewer before a final determination. Denials will not be considered evidence of negligence but rather noncompliance with insurance standards. Vascular surgeons who provide appropriate care will not be required to undergo a similar review in the following year. Providers who fail such a review will undergo further spot checks at six monthly intervals until they are seen to comply with appropriate standards of care. Continuing abusive behavior may warrant exclusion from Medicare or the insurance carriers’ panel. The ACVES, being primarily responsible for this program, will market it to the various insurance carriers who, if they agree to participate, will pay a premium over the costs to be divided by the ABVES and the ACEVS.
The program has multiple benefits. The ACVES and the ABVES will be provided with a source of income that will keep these organizations solvent for the foreseeable future. Payers will see a significant reduction in the cost of provider oversight, a drastic reduction in the number of costly unnecessary procedures, and, by improving the health of their members, a further reduction in expenses. Vascular surgeons will not have to put up with time-consuming, expensive and frustrating PAs. Most importantly, they will be able to advertise to patients that they voluntarily agreed to a program of oversight and that their services have met the highest standard of peer review. Further, insurance carriers choosing providers for their panel will likely seek only those who are part of this program. This will guarantee that vascular surgeons are once again promoted as the appropriate providers of vascular services. Most importantly, the standard of care for vascular patients will be vastly improved. I am hopeful that eventually cardiology and interventional radiology will partner with us to improve the vascular health of the nation.
References
- InterQual. Evidence-Based Criteria/Guidelines. Utilization Management. InterQual. Change Healthcare
- Society for Vascular Surgery appropriate use criteria for management of intermittent claudication. Journal of Vascular Surgery volume 76, issue 1, p 3–22 April 2022
- ACC/AHA/SCA/SIR/SVM 2018. Appropriate use criteria for peripheral arterial intervention. Journal of the American College of Cardiology volume 73 No2 2019
- Dietzek A. Vascular surgery is the best kept secret in medicine and my thoughts on how we can change that. Journal of Vascular Surgery Vol. 69 Issue 1 p 5–14 Published in issue: January, 2019
RUSSELL H. SAMSON is president of The Mote Vascular Foundation and past medical editor of Vascular Specialist.











