A retrospective review of a rare set of pediatric bone tumor resection cases with significant blood vessel involvement has demonstrated 100% limb salvage and 0% local recurrence.
The 14-year experience involved 117 cases treated at Louisiana State University (LSU) and Tulane University in New Orleans by a vascular and pediatric orthopedic surgical team. First-named researcher Malachi Sheahan III, MD, chief of vascular surgery at LSU, said the series likely represents the largest known set of its kind in the literature, demonstrating how a multidisciplinary team can tackle pediatric bone tumors “with minimal blood loss, excellent limb salvage and low rates of local recurrence.”
Data on the findings were revealed during the 2022 annual meeting of the Southern Association for Vascular Surgery (SAVS) in Manalapan, Florida (Jan. 19–22).
Sheahan and colleagues started to take part in pediatric bone tumor cases—comprising osteosarcomas, osteochondromas and aneurysmal bone cysts—in 2006, later discovering no apparent reports of the value provided by vascular surgery in their execution.
Sheahan told SAVS attendees how the series counted 57 osteosarcomas, 51 osteochondromas and nine aneurysmal bone tumors through 2019, and provided an insight on the techniques utilized in order to arrive at the outcomes he reported from the podium. The average age of the population of patients in the study was 11.6, with 56% of them being female. The patients were derived from across the U.S., with their varied chemotherapy and radiation therapy treatment regimens accounting for a central weakness of the dataset, he pointed out.
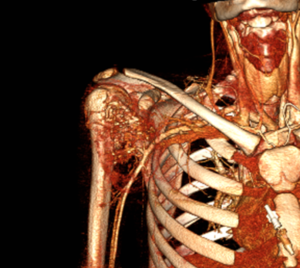
When dealing with osteosarcomes, Sheahan explained, “it’s our job to find out what’s tumor and what’s inflammation. With every single one of these, it looked like the blood vessels were involved based on the preoperative MR [magnetic resonance], but in most cases you can develop a plane between the tumor and the vessels. If you can’t, then you ligate the vessels and reconstruct. It’s cancer, so you don’t leave anything behind.”
Sheahan said his team’s approach involves securing the neurovascular bundle as a unit to then achieve exposure to the bone. The technique used when dealing with osteochondromas is similar to that used with osteosarcomas, he added. “With aneurysmal bone cysts, in the literature these have a very high rate of recurrence,” Sheahan continued. “They’re not malignant but they are very, very vascular and devastating to the bone involved. You can’t resect the entire bone, so either you do curettage or embolization. Our technique is to do both. The literature reports a 30% recurrence rate, and I’m going to report a 0% recurrence rate with this technique.”
Speaking from the conference floor, Martyn Knowles, MD, a vascular surgeon at UNC Health Care in Raleigh, North Carolina, the designated discussant for the paper, queried Sheahan on how the patient population was followed and how decisions were made over when and when not to resect. “We follow them for life—we don’t have literature on kids and reconstructions to let us know when it’s OK to let them go, ” Sheahan said.
“The technique is as much art as science. At the start of this approach, we started sending a lot of frozen sections of tissue off to see if there was tumor present. That led me to be more aggressive with the vessel salvage and identifying what’s inflammation and what’s tumor. That’s easier to do in situ than radiographically, I think,” he added.












