Physician-sponsored Investigational Device Exemption (IDE) trials have an important role to play in the continued development and refinement of aortic endovascular devices, attendees of a panel session on aortic device regulation heard yesterday.
The session, taking place Wednesday lunchtime, set out the various Food and Drug Administration (FDA)-mandated pathways that a device must follow before it can enter the market, as well as looking at the involvement of vascular surgeons in this process. Speakers from the FDA outlined the agency’s priorities in ensuring the safety of devices that are approved for use, while balancing the need to encourage innovation.
Considerable innovation has resulted from physician-sponsored IDEs focused on treating patients with complex aortic aneurysms. “There have been substantive learnings that have really contributed tremendously to the development of future clinical studies, to device design modifications and really have helped the endovascular aortic space move forward for many years,” Ronald Fairman, MD, FDA’s Vascular and Endovascular Devices (VEDT) medical officer, and a former SVS president, said during his presentation examining the role of physician-sponsored IDEs.
Fairman outlined the similarities and differences between corporate and physician-initiated IDEs, including the circumstances in which the FDA may recommend the submission of an IDE, citing the example of the use of physicianmodified devices or where a commercial device is routinely being used for a new indication.
“It is important to acknowledge, the FDA does not regulate the practice of medicine,” said Fairman. “If you are modifying a device to save someone’s life, the FDA does not get involved in that. You do not need a investigator-sponsored IDE for that.
“On the other hand, if you are modifying a commercial aortic device or using a commercial device for a new indication and you are doing it routinely, and you are collecting safety and efficacy data to see if it works, we would continue to recommend a sponsored-investigator IDE.”
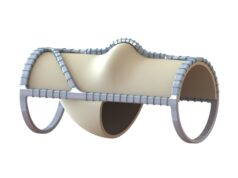
Gustavo Oderich, MD, professor of surgery and chair of vascular and endovascular surgery at the University of Texas Health Science Center at Houston, shared his considerable experience in physician-sponsored IDEs, and outlined several important developments to have emerged from this setting, in particular in the development of fenestrated-branched endovascular technologies.
“Physician-sponsored IDEs provide a safe venue for continued access, innovation and refinement of endovascular techniques,” Oderich said, setting out several scenarios in which these trials add value. “These often represent the highest level of data for the specialty, and even after a device is approved new iterations will continue to be needed.”
FDA medical officer Robert Craig, DO, outlined the agency’s approach to postmarket data collection and underscored the importance of vascular surgeons participating in the postmarket clinical studies that FDA requires for aortic endografts as a condition of premarket approval (PMA) application.
To conclude the session, moderator and FDA VEDT medical officer Robert E. Lee, MD, outlined the regulatory requirements for medical device event reporting. He underscored the importance of vascular surgeons voluntarily reporting the adverse medical device events encountered in practice using the FDA MedWatch system