Over the course of more than a year, diversity, equity and inclusion (DEI) have been brought into sharp focus by a compendium of events inside and outside of medicine. As U.S. society has reckoned with the socioeconomic and cultural consequences of racial and gender disparities, so too has vascular surgery.
Over the course of more than a year, diversity, equity and inclusion (DEI) have been brought into sharp focus by a compendium of events inside and outside of medicine. As U.S. society has reckoned with the socioeconomic and cultural consequences of racial and gender disparities, so too has vascular surgery.
Vascular surgery has been at the vanguard as disparities in vascular disease and outcomes have sharpened minds on the need to address societal imbalances.
At this year’s Vascular Annual Meeting (VAM), a special DEI session has been convened, featuring a broad cross-section of science delving into vascular disease disparities across racial, ethnic and gender lines.
Moderated by Ronald L. Dalman, MD, the outgoing Society for Vascular Surgery (SVS) president, Vincent Rowe, MD, chair of the SVS DEI Committee, and Bernadette Aulivola, MD, a member of the committee, the session is being kicked off with an experiential talk to be delivered by Lee Kirksey, MD, the Walter W. Buckley-endowed vice chairman of vascular surgery and co-director of the Center for Multicultural Cardiovascular Care at the Cleveland Clinic in Cleveland, Ohio.
Direct and indirect effects of race and socioeconomic deprivation on vascular surgical presentation and outcomes
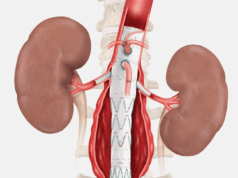
Chloe Powell, MD, an integrated vascular surgery resident at the University of Michigan in Ann Arbor will present on the association between race and socioeconomic status, as measured by the area deprivation index (ADI), on outcomes following vascular surgery procedures. Powell et al used a statewide quality registry in order to investigate patients who underwent abdominal aortic aneurysm (AAA) repair, open lower-extremity bypass, carotid endarterectomy and stenting from 2012 to 2019. The study demonstrated, the researchers will reveal, that Black race and socioeconomically disadvantaged patients “tended to have more advanced peripheral vascular disease on initial presentation with less preoperative medical optimization, indirectly leading to increased morbidity and death.”
Racial disparities in treatment of ruptured AAAs
Thomas F. O’Donnell, MD, a vascular fellow at Beth Israel Deaconess Medical Center in Boston, will deliver data on transfer rates, turndown rates, and outcomes in Black vs. white patients presenting with ruptured AAA (rAAA) in two large databases. O’Donnell and colleague examined all repairs of rAAA in the VQI from 2003 to 2020. “Black patients with rAAA are poorly served by the current systems of interhospital transfer in the U.S. as they less often undergo transfer prior to repair,” O’Donnell will tell VAM attendees. “Although postoperative outcomes appear similar, this may be false optimism, as Black patients, especially the underinsured, are more often turned down for repair even after adjustment. Significant work is needed to better understand the reasons underlying these disparities and identify targets to improve the care of Black patients with rAAA.”
Gender disparities in major depression among patients with PAD and associations with mortality
Gloria Y. Kim, MD, a vascular surgery resident at the University of Michigan in Ann Arbor, will tell VAM that depression is associated with adverse cardiovascular events but is seldom included in risk assessments among patients with peripheral artery disease (PAD). She will deliver findings that emerged from the hypothesis that depression would influence mortality among patients with PAD. Kim and colleagues explored the prevalence of major depression stratified by race and gender, and associations with mortality. The researchers analyzed outpatients enrolled in a cardiovascular risk cohort study from May 2019 to December 2020. They found that major depression is common among patients with PAD, “and prevalence among women was nearly double that of men.” They will conclude: “Depression is associated with mortality among patients with PAD who are not frail. Combining [major depressive disorder] with more traditional comorbidity parameters may improve risk assessment in PAD.”
‘Rupture before the age of AAA screening—another example of disparities in vascular surgery?’
“ADI is a validated measure of socioeconomic disadvantage at the neighborhood level and is increasingly used to assess disparate outcomes across a broad variety of disease states,” Amanda R. Phillips, MD, a resident at the University of Pittsburgh Medical Center, will inform VAM attendees. “Cardiovascular diseases present earlier among minority and socioeconomically deprived patients. Screening at 65 years of age, diagnosis, and elective repair are vital in mitigating the risk of rAAA; however, the association of ADI with rAAA is poorly understood.” This was the backdrop for a retrospective observational study of patients who underwent emergency surgery for rAAA at a multi-hospital institution from 2003–2019 by Phillips and colleagues. They probed patients transported via air ambulance “as most representative of a wide variety of urban and rural communities.” The research team discovered that patients with rAAA were more likely to reside in more disadvantaged neighborhoods, in part concluding that “the most disadvantaged patients presented with rAAA 2.7 years younger than those from less deprived areas” and “one third of disadvantaged patients ruptured before age 65— the recommended age for initiating screening.”
Disparities of healthcare access among Hispanics at risk of lower-extremity amputation
Tze-Woei (Kevin) Tan, MD, associate professor of surgery at the University of Arizona College of Medicine in Tucson, will deliver findings demonstrating that Hispanics are disproportionately more likely “to not seek or delay medical care than their counterparts due to socioeconomic reasons.” This could be leading to disparities in lower-extremity amputation, Tan and colleagues concluded after carrying out a study of Hispanic and non-Hispanic patients in the National Institutes of Health (NIH) All of Us Research Program to identify participants with PAD or diabetes. The analysis included 432 Hispanic participants and 3,219 non-Hispanic participants—2,551 of them white, 587 African American, 82 Asian, and 79 listed as “other.” After multivariable analysis, the researchers’ results showed that Hispanic participants were significantly more likely to delay medical care (p<0.05) due to employment, childcare issues, worries about paying, and nervousness about seeing a doctor than non-Hispanic participants.
When: Friday, Aug. 20, 10 a.m.–11 a.m. Special Session: Diversity, Equity & Inclusion