
Looking to the future, genetic testing may play a role in guiding the intensity of therapeutic interventions and preventive strategies in patients with venous disease. This finding comes from a case-control study on the clinical implications of genetic variation of venous stasis ulceration, presented by lead researcher, Rabih Chaer, MD, at the 2022 annual meeting of the American Venous Forum (AVF) held Feb. 23–26.
Venous stasis ulcers are the most common cause of non-healing lower-extremity wounds and can persist despite adequate pressure and ablation therapy, Chaer, chief of vascular surgery at UPMC Presbyterian in Pittsburgh, explained. “Although great progress has been made in wound care and treatment regimes, the response remains variable, and, regardless of the clinical strategy used, it is evident that there is a lot of variability in the outcomes of patients who present with similar disease patterns.”
Few institutional theories have examined the role of single gene polymorphism independent genesis of venous stasis alteration, he said, and the most recently published series have typically focused on a few target genes and were limited by small sample size.
Chaer’s case-control study, funded by the AVF and AVF-JOBST Clinical Research Grant, held the hypothesis that genetic profiling of venous status ulcers can potentially stratify patients according to their potential for disease progression, healing, and also guide them through preventive strategies and levels of therapeutic intervention. Chaer relayed that the study’s purpose was to determine whether single nucleotide polymorphisms (SNPs) in select genes can affect ulcer formation or healing.
He noted that genotyping was carried out for 19 targeted SNPs associated with wound healing or thrombophilia, using Taqman SNP genotyping technology. Of those, five of the markers were validated using real-time PCR to ensure genotype clustering. Repeat samples were performed at the initial run and multiple replications were performed to ensure genotype accuracy.
Data related to the patients’ venous disease were prospectively collected for two years and included demographics, ulcer information and clinical management. Additionally, logistic regression models were used to identify factors associated with ulcer formation and healing using a cut-off p-value of 0.2 to capture trends. He explained that the primary endpoints were ulcer healing or ulcer recurrence, and the secondary endpoints included the genetic association with ulcer healing, and time for healing and recurrence. The researchers also looked at genotype and phenotype correlation for the variables, and analyzed the clinical variables in conjunction with ulcer healing and recurrence.
Chaer said that MMP12 was found to be significant in the study as associated with inflammation. Another is associated with fibroblast activity, such as GP6. F13A1 (factor 13A1) was associated with thrombophilia.
The study enrolled a total of 377 patients: 23% (n=85) CEAP 5, 33% (n=126) CEAP 6, and 44% (n=166) controls (50 or older). All patients underwent a systematic evaluation of their superficial venous system. The average patient age was 63±12 years, 13.3% (n=50) were African Americans, and 56% (n=211) were females. Chaer noted there were more females in the patient control group. The average follow-up time for CEAP 5/6 patients was 19±10 months (range: 0–50 months; median: 23 months). CEAP 5/6 patients had a lower incidence of the GP6 SNP (rs1654416).
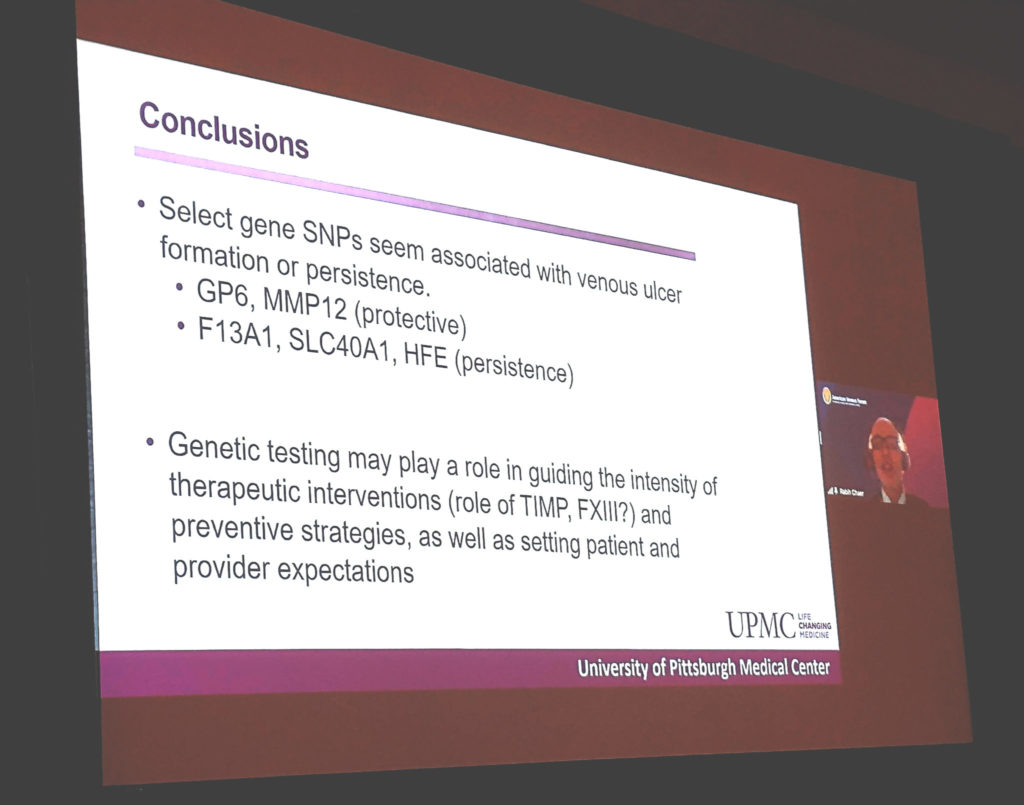
Recalling the results, Chaer said that in the CEAP 5 group, 17.1% (19/111) of limbs had ulcer recurrence (average time period to ulcer recurrence was 13.62 months). In the CEAP 6 group, 46.9% of limbs (n=67/143) healed, 32.2% (n=46) improved, and 21% (n=30) worsened (mean time to ulcer healing was 7.38 months). On multivariate logistic regression, GP6 (rs1654416) and MMP12 (rs651159) SNPs were protective against ulcer formation, whereas F13A1 (rs5985), SLC40A1 (rs11568351), and HFE (rs1800730) were associated with ulcer persistence. GP6 was the only gene which was found to be significantly less expressed across the cases.
“Select gene SNPs seem associated with venous ulcer formation or persistence and genetic testing may play a role in guiding the intensity of therapeutic interventions and preventive strategies, as well as patient and provider expectations,” Chaer concluded.












