
“Deep vein arterialization is safe and technically feasible,” Peter Schneider, MD, a professor in the division vascular and endovascular surgery at the University of California San Francisco, said during a recent presentation on 12-month data from the PROMISE I early feasibility study of the LimFlow system (LimFlow) in no-option chronic limb-threatening ischemia (CLTI) patients.
He was speaking during a late-breaking trial session at LINC 2021 (the Leipzig Interventional Course)—held online from Jan. 25–29—that saw key updates on below-the-knee (BTK) interventions brought in the spotlight.
PROMISE I is an early feasibility study launched in mid-2017, with the purpose of establishing the clinical safety of the LimFlow system in order to move into a pivotal study, identifying and addressing operator challenges when using the device, and determining patient and therapeutic parameters that impact performance.
Schneider informed LINC listeners that conducting an early feasibility study has the advantage of enabling the optimization of operator technique, and developing and refining protocols, including patient screening, wound analysis and patient follow-up.
Technical procedural success was 97%.
Amputation-free survival at 30 days was the primary safety endpoint; this was 70% at 12 months. “These are ‘no-option’ patients, as determined by an independent review committee, who would have gone on to amputation in the vast majority,” he said, contextualizing the results.
Breaking down the amputation-free survival metric at 12 months, which is a compound measure including survival and freedom from amputation, he shows that at one year, survival was 91%, and freedom from amputation was 77%. Following his announcement that limb salvage for patients with “no-option” revascularization was achievable in 77% of patients at 12 months, the speaker concluded that lesion from this initial trial will be “incredibly valuable” moving forward.
Referring to the wound status over time for patients treated with LimFlow in this early feasibility study, Schneider showed that at 24 months, 88% of wounds were either healed or healing.
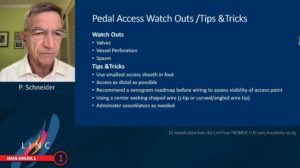
Outlining the lessons learned from this study, he commented: “Inflow arterial lesions must be treated aggressively. Pedal venous anatomy access should be obtained as distally as possible. Pre-existing arterial vessels should be maintained to the extent possible because it takes some time for the venous arterialization to mature.”
“We continue to gain insights into technical issues and methods to improve outcomes for these patients,” Schneider closed.












