This advertorial is sponsored by Inari Medical.
For Joseph M. Liechty, MD, a vascular surgeon with Texas Vascular Associates in Plano, Texas, the emergence of the RevCoreTM and VenaCoreTM devices (Inari Medical) have helped broaden his treatment strategies for advanced venous disease patients in whom options were previously limited. Liechty, who operates in the Dallas-Fort Worth (DFW) metroplex, sees a significant number of patients living with the long-term sequelae of deep vein thrombosis (DVT), especially those with symptoms of post-thrombotic syndrome (PTS).
Here, he describes how he has harnessed the RevCore thrombectomy catheter to tackle in-stent thrombosis and the VenaCore thrombectomy catheter to address challenging venous occlusions, as he builds a venous practice that reaches beyond best medical therapy with a limited suite of interventional tools. These new thrombectomy devices, Liechty explains, have helped him reach a community in need of alternatives with enduring results.
Can you describe how your venous practice has evolved since you started to see patients in the DFW metroplex?
Venous patients make up about 30% of all the cases I do now, with acute referrals coming from emergency departments (EDs) and hospitalists from multiple healthcare systems in the area, and from outpatient clinics dealing with more chronic DVT and symptomatic venous obstructions. When I first came here, I did a lot of ED and intensive care unit talks and I visited primary care, wound care, hematology/oncology and cardiology practices. I did a lot of promotion, case sharing, and awareness work because the technology was so new.
There has been a long-standing paradigm of treating venous disease extremely conservatively that is not easy to change. Something that has been helpful when speaking to colleagues is to have trials and data to show them, as well as case presentations.
In what ways have RevCore and VenaCore grown your practice?
Prior to the introduction of RevCore, there was a certain period in which a thrombectomy needed to be done before the clot in the stent became impossible to remove and would require a new stent to be placed inside the old one. The only real option was to go in with some kind of aspiration tool to remove the thrombus or use thrombolytics; however, neither of these options were consistently effective in cases where the thrombus had been present for perhaps a couple of weeks, and so it was a pressing matter to get the thrombectomy done as soon as possible. With the RevCore device, that sense of urgency has been removed. We have the liberty to go in a little bit later. More importantly, if a patient should present late with a thrombosed stent, we don’t have to say, “There is nothing we can do.”
Additionally, prior to RevCore, if you couldn’t get the clot out when it was fresh, you didn’t really have any other choice than to place another stent. RevCore gave us an option to remove thrombus of varying chronicity from an existing stent and hopefully limit the need to place another.
What has been your experience offering patients treatment with the RevCore and VenaCore devices when previously they couldn’t get an interventional option?
We have had a lot of success. We haven’t had many cases where there has been thrombus that has been resistant to these devices. I have found VenaCore to be especially useful in the common femoral vein, where perhaps there would be concern for having to stent across the infrainguinal ligament, even though this is well-tolerated when I’ve done it.
For clotted stents, the only option was to aspirate whatever could be removed, perform balloon angioplasty, and then possibly place more stents, leading to patients with a couple of layers of stents if they had experienced more than one clotting episode. RevCore allows you to clean out stents, which has decreased my need to re-stent.
What would you tell your peers about building an advanced venous practice?
There are a lot of upsides. We deal with patients who have problems for which they have been told there aren’t any good solutions. In the vascular world, DVT is different because the disease process skews toward a younger population compared to arterial disease. We can improve the quality of life for people who are still trying to work and support a family, for example.
Advanced venous cases require considerable planning in terms of anatomy, thrombus distribution, pre-existing stents and/or filters, and available access points, as well as which devices are available. We have seen very grateful patients for whom previously there wasn’t anything we could do other than offer compression stockings and anticoagulation.
If you are just starting out with these devices, perhaps an ideal patient might be one who has a unilateral problem and no thrombotic history. For more advanced cases, I favor general anesthesia because these cases can take a few hours, and having multiple access sites could be uncomfortable for an awake patient.
Can you break down how RevCore fits into your surveillance of patients who have had a stent placed?
I schedule regular surveillance on all the iliac vein stents I implant—I routinely follow up with these patients at four weeks, three months, nine months and then annually— and occasionally we’ll see stents that appear to be occluding, developing a lining on the inside that narrows the flow lumen.
There is a subset of patients whose stents will eventually go on to occlude and they remain asymptomatic. This is probably because they have managed to develop collaterals that are sufficient during that time. But I also have patients who have a stent that is starting to occlude, and they are beginning to have swelling and pain in their leg. Those are the patients who don’t have collaterals yet, or maybe they are always going to be dependent on their stent. These are the patients on whom I would intervene early. Essentially, my strategy is based more on how the patient feels and how the leg looks rather than whether there is some narrowing on ultrasound. That shouldn’t be the deciding factor.
Case report
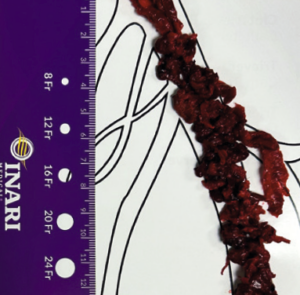
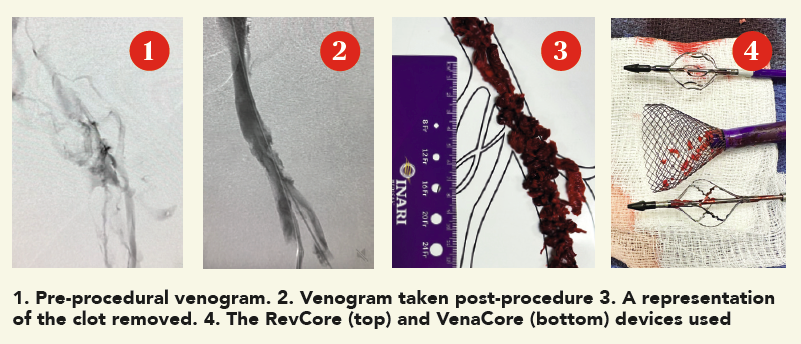 A man in his late 60s with a left iliac vein stent and revision two years prior was referred for consultation. The patient discontinued his anticoagulation two months before he was referred for consultation for severe left leg swelling. Duplex ultrasound confirmed a reoccluded left iliac venous stent. The decision was made to intervene with mechanical thrombectomy.
A man in his late 60s with a left iliac vein stent and revision two years prior was referred for consultation. The patient discontinued his anticoagulation two months before he was referred for consultation for severe left leg swelling. Duplex ultrasound confirmed a reoccluded left iliac venous stent. The decision was made to intervene with mechanical thrombectomy.
Procedural overview
Access was obtained in the superficial femoral vein and right internal jugular (IJ) vein under ultrasound guidance. A venogram demonstrated significant thrombus in the common femoral vein, profunda and extending into the external iliac vein. A .035” guidewire was inserted into the femoral vein and externalized through the access sheath. A ProtrieveTM sheath (Inari Medical) was inserted over the wire into the right IJ vein and advanced into the inferior vena cava. Next, the Triever20 catheter (Inari Medical) was inserted over the wire and directed to the profunda and common femoral vein. Aspiration with the Triever20 removed acute and sub-acute thrombus. Organized material could not be removed with aspiration. RevCore was then inserted over the wire into the occluded stent. Multiple clockwise and counterclockwise turns in conjunction with scrubbing the element within the stent resulted in successful clearance of nonacute thrombus. VenaCore was then introduced through the Protrieve sheath to clear the common femoral vein. Completion venogram demonstrated brisk cephalad flow. Total procedure time was 90 minutes.
DISCLOSURE: Joseph M. Liechty is a paid consultant of Inari Medical. All views and opinions expressed here by Liechty are his own and do not represent those of Inari Medical.
Indications For Use: The RevCore Thrombectomy Catheter is indicated for (1) The non-surgical removal of thrombi and emboli from blood vessels. (2) Injection, infusion, and/or aspiration of contrast media and other fluids into or from a blood vessel. The RevCore Thrombectomy Catheter is intended for use in the peripheral vasculature. The VenaCore Thrombectomy Catheter is indicated for (1) The non-surgical removal of thrombi and emboli from blood vessels. (2) Injection, infusion, and/or aspiration of contrast media and other fluids into or from a blood vessel. The VenaCore Thrombectomy Catheter is intended for use in the peripheral vasculature. The Protrieve Sheath is indicated for use as a conduit for the insertion of endovascular devices into the vasculature while minimizing blood loss associated with such insertions. Triever Catheters are indicated for (1) The non-surgical removal of emboli and thrombi from blood vessels (2) Injection, infusion, and/ or aspiration of contrast media and other fluids into or from a blood vessel. Triever Catheters are intended for use in the peripheral vasculature and for the treatment of pulmonary embolism. Triever Catheters are also intended for use in treating clot in transit in the right atrium, but not in conjunction with FlowTriever Catheters.
Caution: Federal (USA) law restricts these devices to sale by or on the order of a physician. Review complete Instructions for Use, Indications for Use, Warnings, Precautions, Possible Adverse Effects and Contraindications prior to use of the product. For all non-Inari products, please refer to complete manufacturer Instructions for Use/ Intended Purpose for complete indications for use, contraindications, warnings and precautions. All copyrights and trademarks are property of their respective owners.
Inari Medical 6001 Oak Canyon, Suite 100, Irvine, CA 92618