This advertorial is sponsored by AOTI.

Until about a decade and a half ago, vascular surgeon Alisha Oropallo, MD, could be counted among the skeptics. Back then, she says, topical wound oxygen therapy for nonhealing vascular wounds did not have much traction in the vascular surgery community. Skepticism was widespread. There was little data behind the technology of the time, and questions lingered over its effectiveness.
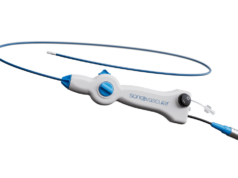
Then along came a new mechanism of oxygen delivery to the wound bed. Data followed, including results from a randomized controlled trial (RCT) showing durable healing in chronic diabetic foot ulcer (DFU) wounds.
The key difference maker, says Oropallo, who is professor of surgery at Zucker School of Medicine at Hofstra University/ Northwell and director of the Comprehensive Wound Healing Center at Northwell Health in New Hyde Park, New York, is the cyclical pressurized oxygen applied directly to sites of wounds by Topical Wound Oxygen (TWO2) therapy.
“It wasn’t cyclical before, there wasn’t 100% oxygen, there wasn’t proof that it was actually penetrating the tissues—I think they were just blowing in oxygen from the outside and there wasn’t really a pump mechanism for the most part,” she explains. “It’s new and different multi-modality functionality in how it penetrates the wound with oxygen.”

For Oropallo, TWO2 use is now routine. With DFU patients who qualify, she starts topical oxygen therapy almost immediately. For patients who she sees with radiation injuries, she almost always refers them for TWO2. And then there are those patients with venous leg ulcers (VLUs), and particularly recurrent VLUs.
A real-world outcomes study, conducted on a very co-morbid diabetic population—similar to the population that Oropallo treats—showed that even in the face of dysvascular function, and in many cases dialysis, this technology can help this particular population achieve successful outcomes and expedite healing of these hard-to-heal wounds. As the data in the study—carried out by Jessica Izhakoff Yellin and colleagues, and published in Advances in Wound Care in 2021—demonstrates, the significance of being able to decrease hospitalizations that prevent amputations in this group of patients with diabetic foot ulcers is life changing for them, Oropallo points out. It also showed that it was economically beneficial for all concerned when this TWO2 therapy can be implemented, she adds.

Oropallo cites a recent VLU case involving a 64-year-old man with a history of multiple deep vein thromboses (DVTs) and Factor V Leiden deficiency. Prior, he had undergone left iliac vein stenting and radiofrequency ablation. The patient had residual deep venous reflux of the femoral vein and recurrent leg ulcerations, despite compliance with compression therapy, says Oropallo. “He received adjunctive therapy, such as skin substitutes,” she explains. “TWO2 was applied with subsequent improvement from baseline [image 1] and over four months duration to closure [2 and 3].”
Oropallo says she deploys TWO2 whenever feasible. “I use it throughout the treatment too,” she continues. “Because a lot of times the patients are only given a few weeks of hyperbaric oxygen therapy through insurance and that’s just not enough. So, I use it adjunctively and concomitantly. I don’t find that they’re mutually exclusive. I think that they can both help to enhance the wound healing, at least from a continuous basis.”

“Some do very well with TWO2,” she adds. “It also depends upon the mental status of the patient too, because if the patient is cognitively impaired, that can change the role of how we use TWO2, because they have to administer it themselves.”
Oropallo says the RCT that evaluated the efficacy of TWO2 in the setting of DFUs represented a gamechanger in the level of evidence behind the therapy. Known as the TWO2 Study, led by Robert G. Frykberg, DPM, it demonstrated that at 12 weeks and 12 months, adjunctive cyclical pressurized TWO2 therapy was superior in healing chronic DFUs compared with optimal standard of care alone. Oropallo believes a similar study carried out in the setting of VLUs and published in the vascular literature might eventually lead to topical wound oxygen therapy forming part of the guidelines.

“The TWO2 Study is one of the strongest manuscripts in the literature regarding Wagner grade 1 and 2 DFUs,” she says. “So, I think that pans out really well for vascular surgery in general. If a DFU is a 3 or a 4, then it is more challenging, but the application may still be there—especially concomitantly with an adjunctive therapy.
“Probably the bulk of vascular surgeons’ work is in the field of foot ulcers, because that’s where they do a lot of the revascularization. Most of those patients are admitted in the hospital; they’re going to be under the vascular surgery service line; they’re not going to be under podiatry. The podiatrist might be seeing them ancillary, but the vascular surgeon is really making all the decisions and seeing the patients every day.”
Oropallo contrasts how vascular surgeons face DFU patients with the current VLU treatment landscape.
“Unfortunately, not many patients with venous leg ulcers get admitted too often at the hospital anymore, but they are routinely seen about 80% of the time,” explains Oropallo. “There’s not a lot of good literature out there on topical oxygen in VLUs. But for patients with hard-to-heal wounds who have been recurrently coming back to the office, I wrap the wounds and apply TWO2 on those patients who really have some challenging wounds that are difficult to heal.”