An emerging endovenous valve formation system designed to treat patients with chronic venous insufficiency (CVI) with evidence of deep venous reflux has demonstrated continual improvement since U.S. investigators started performing clinical cases with the device 18 months ago, according to recently presented early data.
The BlueLeaf procedure, currently undergoing clinical research worldwide, has shown a rate of 90% technical success among the first 10 patients treated in the U.S., William Marston, MD, one of the INFINITE-US early feasibility study investigators, told the 2022 annual meeting of the American Venous Forum (AVF) in Orlando, Florida (Feb. 23–26).
These data are part of a total of 30 patients treated at sites worldwide, demonstrating a 93% technical success rate of forming at least one valve, said Marston, who disclosed a consultancy relationship with InterVene, the company behind the BlueLeaf device.
Enrolled patients, classed as C5–6 on the CEAP (Clinical-Etiological-Anatomical-Pathophysiological) classification of disease severity, all had significant deep vein reflux in two main segments between the knee and the common femoral vein, adequate inflow and no acute deep vein thrombosis (DVT), Marston, the vascular surgery division chief at the University of North Carolina at Chapel Hill, explained.
Thus far, all subjects in the study have had a maximum of two valves formed using the device—most performed on the right leg and all monocuspid valves (Food and Drug Administration [FDA] approval has now been granted to form bicuspid valves). The patient pool has a mean age of 59, presented with a venous clinical severity score (VCSS) of 15, and 70% had a previous history of DVT (six on the ipsilateral limb).
Marston told AVF attendees how the U.S. investigators had achieved success in nine out of the 10 patients, with the mean number of leaflets formed standing at 1.7. He further noted how procedure time was currently decreasing, explaining how the system requires a period of adjustment as physicians adapt to patient and equipment positioning. Marston pointed out two minor device deficiencies that did not lead to any complications.
In terms of VCSS among the first six subjects with follow-up out to 12 weeks, investigators saw a mean decrease of 2.3, he said, though he cautioned the early-stage nature of the data. Marston reported no major adverse events, one partial valve pocket thrombosis at one day and one partial distal intraluminal thrombosis. Both were asymptomatic and no longer seen after 30 day duplex follow-up, he added.
The process behind the development of the BlueLeaf system—which gained FDA Breakthrough Device designation late last year—”has been under evolution such that we’re just starting to do bicuspid valves and, in fact, we are scheduled to do the first one in the U.S. next week,” Marston said. “The device we are using today is quite different from the one we used 18 months ago.”
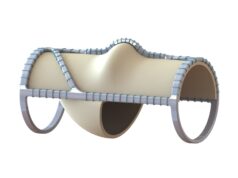
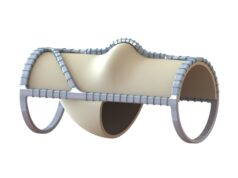
The system involves retrograde access; a high pressure balloon expanded to force the deck of the device up against the vein wall; an advanced needle that enters the vein wall and hydrodissects a flap; and then a nitinol dissector advanced into the flap, expanding and deepening the formation to create a valve cusp.
Improvements made to the latest generation of the device means the valve cusp formed has more depth and a deeper capture of blood after creation, Marston elaborated. Additionally, “the device balloon has been strengthened to help puncture post-thrombotic veins, as most of the patients enrolled are post-thrombotic.”
Marston drew attention to one of the study cases with one year of follow-up to demonstrate the BlueLeaf system’s evolution. The 53-year-old male patient, who had two monocuspid valves created, showed no DVT through 365 days follow up and a VCSS improvement from a baseline of 9 to 6. Marston noted how the valve cusp still showed some motion at one year compared to initial formation. “We’d like to see more but this was with a very early version of the device,” he said. “The cusps are now deeper and wider and hopefully will move better at 365 days than we see here. But this patient did have a well-preserved improvement in VCSS.”
Concluding, Marston told the AVF meeting the BlueLeaf procedure “is technically feasible,” capable of forming valve cusps and under “continual improvement.” “The cusps we are forming today are much better than they were a year ago,” he said, pointing to an “exciting” future as study investigators progress into bicuspid valve formation and the hope of greater luminal coverage.