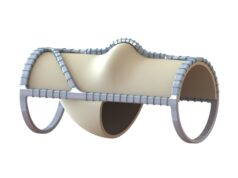
A prospective, multicenter study involving the Covera vascular covered stent (BD) has confirmed the benefits of immediate, post-percutaneous transluminal angioplasty (PTA) placement of the device in treating arteriovenous graft (AVG) venous anastomotic stenosis when anatomically and clinically suitable.
Writing in the Journal of Vascular and Interventional Radiology (JVIR) on behalf of the AVeVA (Arteriovenous stent graft in the treatment of stenosis at the graft-vein anastomosis of AV graft circuits) study investigators, Bart Dolmatch, MD, an interventional radiologist at Palo Alto Medical Foundation, Mountain View, California, and colleagues report a 30-day freedom from safety-related events of 96.4% and a six-month target lesion primary patency (TLPP) of 70.3% with the Covera stent.
The authors begin by noting that, as per three prospective, multicenter, randomized trials, placement of a covered stent has previously led to statistically superior TLPP rates compared to PTA alone in restoring flow and maintaining hemodialysis access.
They add that the current study, AVeVA examined a self-expanding nitinol covered stent (Covera) that is more flexible than the device used in two of those prior studies (Flair, BD).
AVeVA study
Between August 2016 and February 2017, 110 patients were treated by investigators across 14 U.S. centers in AVeVA—a single-arm, investigational device exemption (IDE) study without a concurrent control. Dolmatch and colleagues—the team of investigators includes vascular surgeons Clifford Sales, MD, and Erin Moore, MD—note that, because prospective trials of previous-generation covered stents had been completed and published, and the devices had been approved by the Food and Drug Administration (FDA) for the indication being studied, pooled mean values from these trials as well as additional published data on the use of PTA alone for hemodialysis graft stenosis were used to develop safety- and patency-related performance goals for AVeVA.
The primary safety endpoint was 30-day freedom from an adverse event involving the access circuit resulting in additional intervention, surgery, hospitalization or death. The primary efficacy endpoint was six-month TLPP, or the interval following treatment until the next clinically driven reintervention at the site of the target lesion or until the AVG was abandoned. Prespecified secondary endpoints included acute technical and procedural success, access circuit primary patency (ACPP), cumulative patency, number of reinterventions, index of patency function (IPF), and adverse events through two years.
Of the 181 patients who gave informed consent to participate, 71 did not meet the study eligibility criteria—with 75% deemed not to have angiographic evidence of ≥50% stenosis and clinical evidence of graft dysfunction—meaning 110 patients (mean age=64.3 years, 54.5% female, mean body mass index [BMI]=28.7kg/m2) were ultimately enrolled and treated with the Covera device. The vast majority (98.2%) had an upper-arm AVG.
New Covera data
The authors detail that the mean anastomotic lesion stenosis at the time of treatment was 71.5%, decreasing to a mean residual stenosis of 21% following PTA predilation. One covered stent was used to treat each study lesion, meaning 110 stents were deployed, and all but two of these were postdilated. The mean residual stenosis at procedure completion was 0.9%, Dolmatch and colleagues report. In all cases, the covered stent was deployed to the intended location and eliminated preprocedural symptoms of access dysfunction—constituting a technical and procedural success rate of 100%. All but two patients (98%) resumed dialysis after the procedure using their AVG.
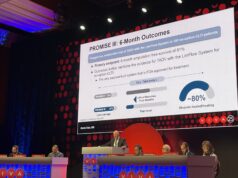
At 30 days, freedom from adverse events was 96.4%. Four patients (3.6%) required additional reintervention and one patient (0.9%) underwent required/prolonged hospitalization. The primary safety endpoint was therefore adjudged to be superior to the performance goal of 88% derived from prior studies and existing literature.
A total of 102 patients (92.7%) were available for the six-month primary efficacy analysis. TLPP at six months was 70.3% among these patients, the authors detail, and this was deemed superior to the prespecified performance goal of 40%. The only observed difference in patient subgroup analyses related to thrombosed AVGs, as those who presented with thrombosis within 30 days of the index procedure and/or at the time of the procedure demonstrated inferior TLPP rates at six months to those in non-thrombosis groups. Dolmatch and colleagues note that reasons behind this are unknown, but the fact this was observed in their study supports the “long-suspected belief” that a thrombosed AVG is more likely to fail due to TLPP loss, even when treated with a covered stent.
Noting secondary endpoint data, which they say should be considered observational and were calculated at predetermined intervals through the end of the study, the authors state that the Kaplan-Meier survival estimates for TLPP were 54.2% at 365 days and 36.9% at 730 days after the procedure, while Kaplan-Meier survival estimates for ACPP were 40.4%, 16.7%, and 7.8%, at 180, 365 and 730 days, respectively. A total of 91 adverse events across 53 patients (48.2%) were reported through 24 months, and 18 patients experienced device- or procedure-related events, meaning 86.3% were free from such events at 24 months.
Concluding messages
The Covera stent did an “adequate job” of maintaining target lesion patency over time, they add, but the “marked” and “ongoing” loss of ACPP (7.8% at 24 months) indicates that—regardless of TLPP improvement with a covered stent—some AVGs may be prone to recurrent stenosis or the development of new stenoses elsewhere in the circuit. The authors state that the 24-month cumulative circuit patency rate of 73.6% further supports this notion, and the finding that TLPP was “acceptable” with covered stent placement. The mean number of reinterventions to maintain patency was 1.6 at the treatment site and 3.6 in the access circuit at 24 months.
Dolmatch and colleagues conclude their JVIR report by noting that AVeVA was designed as “a first-in-human look at the Covera covered stent” in treating AVG venous anastomotic stenosis—and it demonstrated rates of freedom from major adverse events at 30 days (96.4%) and TLPP at six months (70.3%) that were both superior to literature-devised performance goals.
They also note, however, that AVeVA is not directly comparable with other, similar trials like FLAIR Pivotal, RENOVA and REVISE, and outline limitations of the current study, such as the inclusion of thrombosed AVGs and non-target stenoses (rather than a more homogenous AVG group), and the potential for an “inherent bias” being created by its single-arm design and the selection of historical studies. “A comparative, powered, randomized study would be needed to determine patency differences between different covered stents within the same demographic population,” the authors add.