The 2024 Southern Association for Vascular Surgery (SAVS) annual meeting (Jan. 24–27) hears three separate talks—two scientific papers and one from an invited guest lecturer—that separately and from different angles checked the pulse of the arteriovenous fistula (AVF)-first era.
Sandwiched neatly between two complementary dialysis access papers on the SAVS 2024 program, a prominent nephrologist and chair of the taskforce responsible for the 2019 update of the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines delivered a point-by-point take down of the myths that she says surround the idea that AVFs are superior to arteriovenous grafts.
Charmaine Lok, MD, a professor at the University of Toronto in Canada, and medical director of the chronic kidney diseases and vascular access programs at Toronto General Hospital, was delivering the Scottsdale, Arizona-hosted meeting’s Jesse E. Thompson, MD, Distinguished Guest Lecture, the first non-surgeon to do so.
Taking attendees on a tour through the literature, she sought to debunk key aspects around why AVFs are accepted as superior to AV grafts, Lok challenged the argument that fistulas last longer than grafts. However, she said, the key data from which that assertion is derived do not compare all fistulas created vs. all grafts created. “They’re comparing fistulas that actually worked to all grafts,” she explained, making it a “flawed, biased analysis.”
After repeating the analysis, she found that after accounting for primary failure, there was no difference between fistulas and grafts—which was “true for both forearm and upper-arm fistulas.”
Lok added, “And when we looked at upper-arm access only, there was no difference between fistulas and grafts, whether or not we include or exclude primary failures.” Randomized controlled trial data tell a similar story, she said. In one, grafts “actually had superior survival [or lasted longer] compared to fistulas for both primary patency as well as secondary patency.”
Turning to the idea that fistulas have fewer complications, Lok pointed to a rare study in this area that focused on infection rates: among 200,000 patients, the investigators found that, between fistulas and grafts, the rate was the same, she said.
Moving on to the similar contention that fistulas require fewer interventions than do grafts, Lok drew on a study she said summarizes the evidence thus far: “Patency outcomes of fistulas and grafts is a trade-off between non-maturation and long-term outcomes,” she explained, also pointing to evidence from a study with follow-up out to six years showing that 50% of fistulas needed more interventions before use versus only 17% of grafts.
As for the proposition that AVFs lower costs, she pointed to evidence that demonstrated fistulas cost less only when the AVF maturation rate was greater than 82%. “We have already shown you that that is not happening—our fistula maturation rate was only about 40%,” Lok noted.
Finally, she rested on the idea that fistulas are associated with lower mortality when compared with grafts. She cited a study that demonstrated mortality risk was best with fistulas compared to catheters and grafts. Ultimately, Lok said, the higher mortality in those subjects was attributed to the higher comorbidity burden of patients receiving these access types. It boiled down to selection bias, she added.
Which led her to two ultimate questions: What do you think of fistulas now? she asked. Are they really that superior?
“It all depends on your point of view,” Lok said. “Fistula-first was a population-based perspective versus the patient perspective. Now, in this new era, we are looking at patient-centered care—and can you really apply a one-sized fits all to vascular access?”
AVFs in the forearm: Unchanged rates
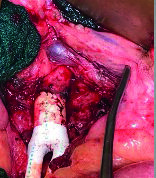
At the podium immediately before Lok, James J. Fitzgibbon, MD, set the tone, as he presented data from a study on temporal trends in hemodialysis access creation in the fistula-first era among a patient cohort who were all recipients of first-time AVF and AV grafts in the upper-extremity.
The Brigham and Women’s Hospital, Boston, resident and colleagues set about answering the central question of whether rates of AVFs in the forearm are increasing. In short, they found that forearm fistulas constituted only a quarter of first-time accesses in the Vascular Quality Initiative (VQI) dialysis access database, with no significant increase seen across the 2012–2022 study period.
Upper-arm AVFs made up 57% of the 52,000 patients included in the retrospective cross-sectional analysis, with 15% upper-arm AV grafts and 1.5% AV grafts in the forearm. “There was no significant change in forearm AVFs across our study period,” Fitzgibbon told SAVS. “The only significant change we did find was there was a decrease in forearm AV grafts.”
Fitzgibbon and colleagues had a particular backdrop in mind as they conducted the analysis: the fistula-first approach described by Lok that was encapsulated in movements to promote autogenous access across the U.S., first with the “Fistula-First” initiative of 2005, and then the “Fistula First-Catheter Last” campaign it morphed into by 2015.
They looked at the impact of the latter by conducting an interrupted time series analysis of the rates of AVFs and AV grafts both before and after it was launched, but they did not detect a significant effect on the rates of AVFs or AV grafts after implementation. However, they did uncover significant increases in upper-arm AV grafts in women, elderly and Black patients, Fitzgibbon added.
“The goal of this project was to broadly report practice patterns across the U.S.,” he concluded. “This is by no means a comment on appropriateness of access; this is not trying to say that every patient should receive a forearm fistula, or is appropriate for a forearm fistula.”
Exploring appropriate access selection
Near the close of SAVS 2024, Bright Benfor, MD, a research fellow at Houston Methodist in Houston, Texas, stepped into the dialysis access fray with a study that compared surgeon choices of AVF to that recommended by an emerging app called “My Vascular Access.”
The program, which grew out of expert consensus and the KDOQI guidelines, is aimed at helping guide the right type of access for patients.
“Two days ago, we heard Dr. Lok talk a lot about the new KDOQI guidelines and how they focus more on a shift from fistula-first to the right access, for the right patient, at the right time, and for the right reasons,” Benfor told attendees.
With that in mind, Benfor and colleagues conducted a review of patients undergoing autologous AVF creation at Houston Methodist to determine how its surgeons’ choices between January and August 2021 held up against the app’s appropriateness rankings, ultimately asking, “Do we need it?”
They looked at 113 accesses performed during the study period. “We can see that there is a high number of radiocephalic fistulas that we created during that time, and we saw the number actually created were statistically significantly higher than the numbers that were recommended,” Benfor said. “Also, in other cases, the app recommended a graft be placed, but our surgeons went ahead and put in a fistula.”
Overall, 61% of the accesses were ranked as appropriate by the app, with 22% deemed inappropriate and 10% intermediate. “There is a significant mismatch between what the app is recommending and access actually created by the surgeons,” he concluded. “One thing we believe influences the choice of access is the level of expertise of the surgeon, which is not taken into account by an app.”