
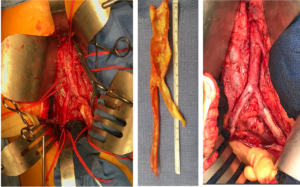
The uncommonly performed aortoiliac endarterectomy—one of the open procedures on which the vascular surgical specialty was founded—provides acceptable durability in aortoiliac occlusive disease patients with smaller native vessels, especially among females, a 25-patient case series review performed at Louisiana State University (LSU) Health Sciences Center in New Orleans has shown.
Results from the analysis, presented at the 2024 Southern Association for Vascular Surgery (SAVS) annual meeting in Scottsdale, Arizona (Jan. 24–27), by Shivik Patel, MD, demonstrated freedom from major adverse limb events of 89% and 81% at two- and three-years post-procedure, while primary and secondary patency out to three years were 86% and 89%, respectively.
The patient sample, dating from 2006–2022, was 72% female with a mean age of 53.6 years. Overall survival was 94%. “Two patients had early postoperative thrombosis, and both of those patients had undergone procedures in an acute limb ischemia type of event,” explained Patel, formerly a vascular surgery resident at LSU and now an attending surgeon at WellSpan Health in York, Pennsylvania, in an interview with Vascular Specialist. “Among the patients who underwent the procedure in an elective circumstance, there was one instance of late reintervention that was needed., but, overall, this series shows pretty durable outcomes after three years.”
A subanalysis involving mean aortic and iliac diameter measurements further demonstrated that the patient cohort had smaller native vessels than the means of a general population, Patel continued.
“We went through all of the patients’ imaging and measured their juxtarenal aorta, their infrarenal aorta, distal aorta and bilateral iliac arteries, as we wanted to compare our group to standard population means for the age group,” he said. “We saw that our aortic diameters and iliac diameters were less than those means.”
Patel conceded study shortcomings, principally the lack of a control group. “Our study involved predominantly females, which could provide some bias in terms of having a mostly female sample, but I think it speaks to the benefit something like this procedure can have in the female population,” he added.
Patel argued that given the surgery’s relatively uncommon use in practice, the 25-patient sample provides a “fairly robust” dataset with which to introduce numbers that suggest a role among a specific patient group.
“We have noticed, especially in my clinical experience, patients in whom we place stents in their smaller vessels, they are not going to have the durability, and, down the road, you’re going to be placing an aortobifemoral bypass,” he noted. “If you have a reason to avoid a large prosthetic graft, as in an aortobifemoral graft, or avoiding femoral incisions, this is a very durable procedure to do if you have isolated aortic and iliac disease, as long as the patient has acceptable operative risk, which if you’re planning on doing an aortic bypass, the risk is more or less in the same vein at that point.”
Patel sees his data set, for a procedure first performed in the early 1950s, and described in a 2006 Annals of Vascular Surgery paper as “almost a lost art,” as a moment for repose.
“This is an interesting opportunity for us to re-evaluate one of the traditional operative techniques that our specialty is founded on and to make sure we don’t forget about procedures like it,” he said. “They may come back to play a role, and aortoiliac endarterectomy is a surgery I think may re-emerge as a more popular option in patients with specific anatomic specifications.”











