Details of a planned pilot study investigating the merits of performing endovascular aortic repair (EVAR) on abdominal aortic aneurysms (AAAs) in office-based labs (OBLs) and other free-standing ambulatory facilities emerged during the recent Critical Issues America annual meeting (April 16–17) held in Miami.
Principal investigator Enrico Ascher, MD, professor and chief of vascular surgery at NYU Langone Hospital-Brooklyn, New York, and director of the Vascular Institute of New York, spoke of a need to re-visit the little-explored prospect during a presentation entitled, “Developing a successful OBL EVAR program: Is it worth it? What does it take?”
Ascher—who disclosed a potential future relationship with medical device maker Endologix in connection with the pilot study—first took attendees on a journey through the development of ambulatory surgical care in the U.S. The OBL concept emerged in the mid-1960s to increase cost-effectiveness and patient comfort, he explained, and the first one opened in Phoenix in 1970. “There are now more than 5,500 centers across the U.S.”
Ascher presented a series of studies demonstrating the shape of the shift away from the hospital to the ambulatory setting. One used Medicare data to show that while the total number of procedures per 100,000 increased little in a five-year period (2006–2011), the number performed in an office environment experienced a 50-fold increase.
Ascher detailed his own experience of office-based surgical practice after peripheral vascular interventions in the OBL began in earnest in 2008. “Our group started fairly early and accumulated an experience that showed that arterial and venous procedures could be performed safely in an office setting,” he said.
From 2011–2015 at the Vascular Institute of New York, Ascher and colleagues carried out 6,201 procedures, 5,783 of them venous, 238 arterial, 129 arteriovenous access, and 51 inferior vena cava (IVC) filters. He reported no mortalities, “very few complications and excellent patient satisfaction.” Further studies covering venous, arterial and vascular access procedures have produced similar findings, he said.
Ascher outlined some of the advantages of office-based surgery, including improved patient satisfaction, the avoidance of unnecessary hospital admission, decreased overall costs, and independence for vascular surgeons. “They may also be lucrative for physicians,” he added.
But there are also some key guardrails, Ascher continued.
“Patient selection, surgeon experience and well-designed safety clinical pathways are crucial,” he said. “Currently, we are reviewing our data with high-risk patients undergoing peripheral arterial procedures in our office.”
So to the key question: What about the performance of EVAR in the OBL?
“This is not an original question, and I’m sure many of you have thought about it,” Ascher told attendees.” He referenced two studies, one showing that median length-of-stay for EVAR was only two days, and another indicating that 92% of EVAR patients are not re-admitted to the hospital within 30 days.
Which raises the pursuit of criteria for EVAR carried out in the office environment that “can identify a sub-group of patients who can do well with 24-hour admission or no admission at all.”
In this vein, Ascher drew attention to two recent studies with contrasting findings. A study carried out by a research group from Buffalo, which was published in the Journal of Vascular Surgery (JVS), “gave a thumbs down” to the idea of EVAR being performed in a free-standing ambulatory facility “because their ability to predict who can benefit from same-day discharge was not great.”
Yet, Ascher pointed out, surgeons from Chang Gung Memorial Hospital at Linkou, Taiwan, performed 168 EVARs in an outpatient facility, mostly under local anesthesia and sedation, reporting zero mortality, 95% same-day discharge, and a 2.4% rate of readmission within 30 days in a paper published in the Journal of Vascular and Interventional Radiology (JVIR)
In the U.S., little data exist to demonstrate that the concept is viable. Ascher argued the time has now come to explore its potential use.
“As far as I know, Stuart Harlin was the first and only surgeon to have performed EVARs in an office setting,” he said. “Although he never published the series of six cases, he did inform me they were selected, easy cases, and that they all did well. The reason he stopped doing them was because he moved from Florida to Texas, and no longer runs an office procedure lab.”
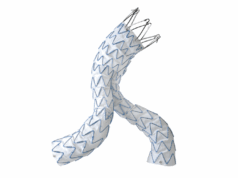
The pilot study planned by Ascher and colleagues is set to involve 10–15 patients who will undergo AAA EVAR using the Alto abdominal stent graft system (Endologix) in the surgical group’s current office operating room (OR). Stringent selection criteria will demand good patient functional capacity, an absence of comorbidities such as uncontrolled hypertension and cardiac arrhythmia, a negative cardiac stress test, and certain anatomical features (for instance: an aortic neck diameter of ≥28mm, angulation of ≤60 degrees and length of ≥15mm; adherence to stent instructions for use [IFU]; no thrombus; minimal calcification; and large iliac vessels free of significant tortuosity or calcification).
“The plan is to attempt a percutaneous approach in all cases,” Ascher commented. “A detailed duplex scan of the common femoral iliac arteries will be performed as an important selection criterion for inclusion in the study.”
The research team hopes to produce early results from the study sometime next year, Ascher added.