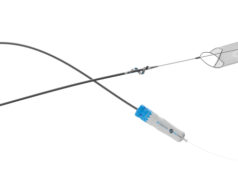
A 74-year-old woman was recently hospitalized for a pulmonary embolus from acute deep vein thrombosis (DVT) of the mildly edematous left lower leg. She had previous DVT in the same leg 10 years ago, wore stockings and was active. She had no family history or evidence of underlying hematologic, or other risk factors. Her son sent me the video, pre- and post-thrombectomy, performed by her cardiologist. It showed non-occlusive bilateral lower-lobe embolization. While I was not privy to many details, her hemodynamic parameters did not appear to me to warrant catheter thrombectomy. She was also advised (I was present as a friend) that she next needed venous thrombectomy of the left leg to “prevent post-thrombotic consequences.” Her next appointment, four weeks hence, was for inferior vena cava (IVC) filter removal. She did well and was discharged on daily apixaban. Was all of this necessary?
Another recent example is that of a vascular surgeon who mandates a full duplex lower-extremity (LE) arterial study, along with a full physiologic LE arterial study, on all patients with possible arterial complaints.
As far as I know, only a few folks who follow the literature on guidelines would question similar decisions—they do not because they wish to keep their heads down, possibly because there is no “quality” issue.
Just like retrospective calculation of deaths from medical “errors,” there is a lot of variation, with even experts disagreeing on what test or procedure is warranted. Unwarranted variation in care is that which “cannot be explained on the basis of illness, medical evidence, or patient preference, but is accounted for by the willingness and ability of doctors to offer treatment.”1
It is estimated that waste or low value (in my opinion, no-value care) in the clinical sense represents about 5.4–24.6% of all healthcare spending in the U.S.2 The largest percentage of this has been attributed to administrative complexity (7%) and pricing failure (6.1–6.3%). Although half of the waste has not been related to physicians, we do not get off easy. Overtreatment (2–2.7%), care delivery (2.7–4.4%), fraud and abuse (1.6–2.2%) and care coordination (0.7-2.1%) are to varying degrees part of our responsibility.2 Retrospectively labeling a clinical decision to treat is many times a judgment call. But, assigning a profit motive to that decision taints all of us.
In a survey of 2,106 physicians from the American Medical Association (AMA) Physician Masterfile, a median of 20.6% of healthcare in the U.S. was seen as unnecessary.3 This included prescription medications (22%), tests (24.9%) and procedures (11.1%). Physicians surveyed estimated that 36% of tests and procedures were unnecessary. Over 70% of them believed that profit was a motivator to perform unnecessary procedures (and I assume tests). Medical specialists were 42.4% of the sample. Granted, the study had limitations, including the fact that most respondents were not in surgical practice and may not have had enough surgical expertise.
Profit implies revenue left over after all expenses are paid to allow paying physician salaries. But if 70% of a group of physicians perceive a profit “motive,” suggesting a conflict of interest in their fiduciary role, is there any practice model that does not create such a conflict? Even the Veterans Affairs (VA) or the foundation physician employment models have conflicts. These can be financial (profit, bonus), productivity targets, promotions, hospital budgets or other incentives that are beneficial to the physician in some way. Every test, patient visit or procedure has represented a financial conflict to varying degrees for decades. However, the work relative value unit (wRVU) compensation model in recent employment agreements creates an ethical challenge for the most principled surgeon. I have written previously about the misalignment of incentives in physician employment by hospitals.4 Employment contracts tie base and bonus compensation to wRVUs and may therefore drive up the volume of services and national healthcare spending, some of which could be wasteful. This occurs at the same time as hospitals are publicly participating in accountable care organizations (ACOs), a shift to “value-based” payments assumed to be cooperating in controlling healthcare spending.
Employer hospitals incentivize maximal physician productivity and stay profitable to service the community, plan future expansion, pay for new technologies, and cover the regulatory and liability onslaught. However, compensating physicians based on pure productivity incentives goes against their responsibility of controlling wasteful spending at the front end. Instead, hospitals are mostly concentrating at the backend by monitoring quality of care, encouraging compliance with national guidelines and specialty self-monitoring. They are correct that physicians do not wish hospitals to interfere with their clinical autonomy. The problem remains that unnecessary care may be done safely, and, since there is considerable grey in guidelines, the amount of wasteful spending goes undetected or ignored. So, is this a stalemate?
The “choosing wisely” initiative has had very limited impact on unnecessary spending. Meanwhile, eliminating all unnecessary care is unlikely, partly because in many cases honest people will differ on the indications of procedures/tests. Several strategies would help, such as better education of trainees and referring physicians with clear guidelines, easier access to outside electronic health records to avoid duplication, and better monitoring of vascular care for appropriateness rather than just quality of care. Rather than pure (100%) productivity, some institutions use formulas to encourage teamwork and reduce competition within the hospital to combat low-value care. As an example, compensation may then be based on the financial performance of the individual (60%), unit (20%), department (10%) and hospital (10%). Self-employed practitioners can come up with a similar model. Quality of care and outcome targets can also be worked into the formula.
For our specialty, barring emergencies or urgent cases, elective procedures can be presented to the practice or division group prior to interventions. For non-elective cases, the indications can be listed and presented to the group after the fact.
For non-interventional procedures such as the vascular lab, we should take responsibility for educating folks about appropriateness and sharing national guidelines, even if other physicians are requesting tests. As medical director of such a lab, ours was probably one of the few departments to decline repeated and inappropriate carotid or venous scans. The sonographers were aware of my criteria for initial or repeat testing. If residents, physician assistants or nurse practitioners who ordered them disagreed with sonographers, they were told to have the attending text or call me if they still wanted the tests. A common example was venous scans of all four limbs for a suspected pulmonary embolus, or a repeat venous scan for major axial lower extremity DVT within a week or two after diagnosis. In many cases, it was obvious that the attending was unaware that the test was requested, and I rarely got contacted. This was not popular, but I did my best to educate.5,6
Again, the lack of “growth” may sometimes cause a problem with hospital administration, so a clear explanation is needed ahead of time. Waste results from “failures of care delivery, failures of care coordination, overtreatment, pricing failures, administrative complexity, and fraud and abuse.”1 We can debate the amount of low-value or unnecessary care and waste, but, in many cases, most of us know it when we see it.
My point is that, even if there is no physical harm, profligate spending justifies a concerted effort to tighten our approach and come up with innovative ways to monitor unnecessary care before our clinical autonomy becomes a dream. I am not suggesting that any—or many—of us are providing low-value care, but the perception is out there. Regardless of the exact percentage of waste we have control over, and whether employed by hospitals or not, it is our obligation to be true to our patients, model our behavior for our students and residents, and sleep well at night.
References
- Wennberg JE. Time to tackle unwarranted variations in practice. BMJ. 2011; 342:d1513
- The Role of clinical waste in excess US health spending. https://www.healthaffairs.org/do/10.1377/hpb20220506.432025/full/
- Lyu H, Xu T, Brotman D et al. Overtreatment in the United States. PLoS ONE 12(9): e0181970. https://doi.org/10.1371/journal. pone.0181970
- Satiani B. Physician incentives may not be aligned with their health system employer. What is a physician to do? Surgery. 2012; 152(5):923–6
- Mouawad NJ, Go MR, Haurani MJ, Moseley M, Satiani B. Elimination of medically unnecessary duplex venous scanning based upon an established algorithm can result in significant cost savings under Medicare for the institution and the taxpayer. Accepted for publication. Journal of Vascular Surgery. Venous and Lym Dis 2015; 3:107–12
- Yoo T, Agrawal R, Braithwaite S, Satiani B, Haurani JH. Four extremity venous duplex ultrasonography for suspected deep venous thrombosis is an anachronism.” Journal of Vascular Surgery: Venous and Lym Dis 2019; 7:325–32
Bhagwan Satiani, MD, is professor emeritus in the division of vascular diseases and surgery in the College of Medicine at The Ohio State University, Columbus, Ohio.