
If you were in the audience at the 2024 Southern Association for Vascular Surgery (SAVS) annual meeting, you might have been taken aback by the presentation from UT Health San Antonio and the San Antonio VA Medical Center, presented by Luke D. Perry, DO, and co-authored by Alissa Hart, MD, Reshma D. Brahmbhatt, MD, and Lori D Pounds, MD: “Work for a dollar get reimbursed a dime: An analysis of the dire need for coders trained in vascular billing,” the paper was entitled.
The authors described that only 42% of the cases for three procedure types were coded correctly, with only 67% of work relative value units (wRVUs) captured. This is a tragedy not just for individual compensation, but also division and department financial accounting, and justification for practice growth, i.e., adding surgeons, advance practice providers (APPs), equipment or otherwise. Our administrators don’t really know what we do on a daily basis, nor do they understand the intricacies of our work and operations. Regardless, the wRVU has now become the currency by which we (“they”) measure our work “effort” and productivity, even though wRVUs do not really measure “physician effort,” the work that we do to take care of patients safely, the education we provide, the research we conduct, and the administrative tasks we must complete by day’s end. Our work is also being measured by other surrogates, including the numerical metrics of number of operations, average case length, on-time starts, and average length of stays. So, while you may feel overworked by the end of the week, you may not be working hard enough according to the administrators, because the measured metrics are not above the median.
In a healthcare economy increasingly reliant upon productivity-based compensation models, knowing the minutiae can mean the difference between getting a bonus or not. Each and every wRVU adds up by the year’s end. Consider codes G2211 and the recent inpatient coding changes: a difference of 0.7 wRVUs per patient encounter could mean more than 360 wRVUs at the end of the year if you have 10 relevant encounters per week. That’s just two a day!
Tracking your “work productivity” is particularly critical if you have coders and billers separate from you and your practice, if you have others who code your procedures, and if you just want to know what your wRVUs amount to.
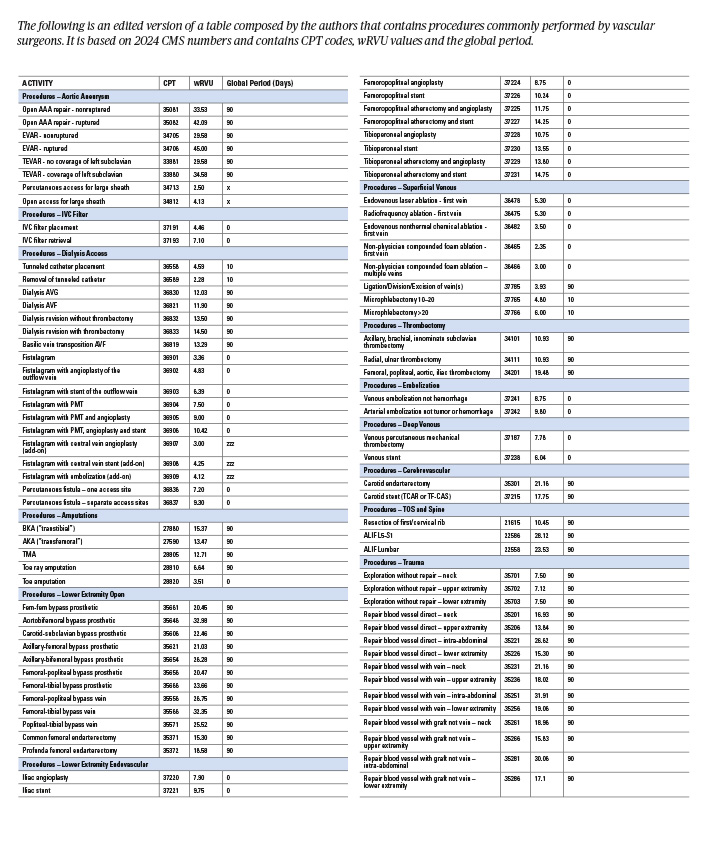
This small group of authors, impressed by the “Work for a dollar get reimbursed a dime” analysis, convened to develop the table provided as a reference for the everyday vascular surgeon. We’ve included the most common procedures that we perform on a daily basis in hopes that we can help our fellow vascular surgeons better account for their daily wRVU earnings. This list will allow you to quickly identify how many wRVUs each procedure carries, and, more importantly, the associated global period associated with a procedure. Did you know that your evaluation and management (E&M) note the day after an inpatient angiogram is a billable encounter? You do now.
The table is based on 2024 Centers for Medicare & Medicaid Services (CMS) numbers, where any and all can look up any procedure at their whim by Current Procedural Terminology (CPT) code. If you just want the wRVU value and the global period, use the first row. The remaining rows are related to reimbursement adjustments based on geographic locations. This table doesn’t even get into the nuances—for instance, adding the diagnostic angiogram codes, if relevant, when you are also doing an intervention, the additional code for brachial plexus decompression during rib resection, modifiers, multiple procedures, etc. It also doesn’t explain the “rules” and allowances of bundled billing versus component billing. But at least it will get you started.
Also captured here is the opportunity cost of your time. So, that challenging open aneurysm repair that takes eight hours is still only about 34 wRVUs. But six or seven vein cases will get you pretty close to that with none of the postoperative headache, and probably less musculoskeletal strain and emotional stress. Not that we’re advocating for patient or case selection based on this; we’re just saying that the next time you get called in to put a stitch in an iliac vein that was traumatized by a laparoscopic port, and you’re done in 30 minutes, be grateful for the quick and easy 26 wRVUs. Knowledge is power. Imagine what you could do with this information. Because, if we don’t know what and how much we do, how can we expect others to know accurately? And, as always, a plug for the Society for Vascular Surgery (SVS) coding course: take your coders, attend yourself. It’s only two days—and an invaluable experience.
 Sherazuddin Qureshi, MD, is a clinical assistant professor of surgery at Northwestern Medicine, Ryan Meyer, MD, is a vascular surgeon at RWJBarnabas Health, Erica Leith Mitchell, MD, is a professor of surgery at the University of Tennessee Health Science Center, Nicolas Mouawad, MD, is chief of vascular surgery at McLaren Bay region, and Issam Koleilat, MD, is also vascular surgeon at RWJBarnabas Health.
Sherazuddin Qureshi, MD, is a clinical assistant professor of surgery at Northwestern Medicine, Ryan Meyer, MD, is a vascular surgeon at RWJBarnabas Health, Erica Leith Mitchell, MD, is a professor of surgery at the University of Tennessee Health Science Center, Nicolas Mouawad, MD, is chief of vascular surgery at McLaren Bay region, and Issam Koleilat, MD, is also vascular surgeon at RWJBarnabas Health.












