During the first day of VAM 2024, the Society for Vascular Surgery (SVS) and American Venous Forum (AVF) have co-sponsored a session on the latest innovations in the delivery of venous disease treatment.
Madhavi Meka, MD, a clinical associate professor at the University of Arizona School of Medicine and vascular surgeon at the Carl T. Hayden VA Medical Center in Phoenix, Arizona, and Faisal Aziz, MD, chief of vascular surgery at the Penn State Health Hershey Medical Center Heart and Vascular Institute in Hershey, Pennsylvania, are moderating a package of presentations (Wednesday, June 19 at 3:15–4:45 p.m. in the West Building, Level 1) focused on recognizing the various patterns of superficial venous reflux and management options, understanding what the most effective treatment for patients with iliac vein disorders is, and increasing knowledge of venous ulcer care and the influence of health inequities.
“Venous disease is more common than peripheral arterial disease [PAD], affecting nearly 30 million people in the U.S. alone,” Meka told VS@VAM. “Twenty-five percent of the global adult population are afflicted with venous reflux disease or a more serious form of venous disease called chronic venous insufficiency. The spectrum of disease ranges from spider veins, telangiectasia, varicose veins, and venous ulcers.”
The initial section focuses on superficial venous disease. Presenting first will be Glenn Jacobowitz, MD, from NYU Health in New York City, who will be discussing thermal ablation options; Karem Harth, MD, from Case Western Reserve University School of Medicine in Cleveland, is up next and will present on non-thermal ablation options; Sherry Scovell, MD, from Massachusetts General Hospital in Danvers, Massachusetts, will finish the superficial venous disease section by discussing sclerotherapy techniques.
The second section focuses on iliac venous stenosis. Arjun Jayaraj, MBBS, from the RANE Center for Venous and Lymphatic Diseases at St. Dominic’s in Jackson, Mississippi, will present on intravascular ultrasound (IVUS) and its importance for deep venous interventions. This will be followed by Misaki Kiguchi, MD, from MedStar Heart and Vascular Institute in Washington, D.C., who will discuss stenting below the inguinal ligament.
The final section of the SVS-AVF session covers venous leg ulcerations (VLUs), starting with William A. Marston, MD, from University of North Carolina at Chapel Hill, North Carolina, who will be presenting on whether deep or superficial interventions should be tackled first.
Meanwhile, Anil Hingorani, MD, from NYU Langone in Brooklyn, New York, will present next on the role of perforator veins and interventions in the context of VLUs.
And finally, the last presentation before the panel discussion will be by Leigh Ann O’Banion, MD, from UCSF Fresno in Fresno, California, who will be discussing health disparities in patients with advanced venous disease.
“Despite advancements in the techniques and procedures, there has been a paucity of literature delineating outcomes, patient satisfaction and improvement in lifestyle,” Meka states.
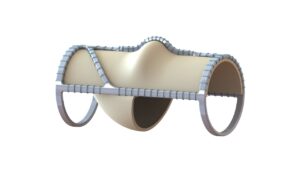
Elsewhere in venous disease developments, on Friday, June 21’s Plenary Session 5 (8–9:30 a.m in the West Building, Level 3, Skyline Ballroom), Cassius Iyad Ochoa Chaar, MD, from Yale School of Medicine in New Haven, Connecticut, on behalf of co-authors Claire L. Griffin, MD, Eric S. Hager, MD, Matthew R. Smeds, MD, and Marc H. Glickman, MD, will discuss the impact of the VenoValve device (EnVVeno Medical) on venous ulcer healing in patients with deep venous reflux.
The presentation features data from the multicenter Surgical Antireflux Venous Valve Endoprosthesis (SAVVE) trial, which highlights the impact of the VenoValve device after one year of implantation for patients treated for venous ulcers.
The SAVVE trial enrolled patients with deep venous reflux and symptomatic advanced venous disease with a clinical, etiological, anatomical, and pathophysiological (CEAP) score of C4b–C6, despite standard-of-care therapy. Patient characteristics were recorded and the revised venous clinical severity score (rVCSS), wound surface area, venous ulcer healing, and improvement defined by the reduction of the area was assessed at the preoperative baseline and at three months, six months and one year. During Chaar’s VAM presentation, updated data on all patients who have reached one-year follow-up will be presented.
The latest results show the trial includes 75 total patients, 41 of whom were treated for venous ulcers and were the focus of the report.
The patient population was majority male (78%) and White (93%), with a mean age of 64. Most of the venous ulcers (70.7%) had a duration of more than one year, while only five patients (12.2%) had venous ulcers that had a duration of less than one month.
The results demonstrate high ulcer healing and reduction of ulcer surface area in a group of challenging patients, the authors will report.
“VenoValve implantation provides sustainable improvement in venous ulcer healing that continues for a year after surgery in patients who have exhausted all current standard-of-care treatments,” the authors will conclude.
Earlier this year at the Charing Cross (CX) International Symposium in London, England, David Dexter, a vascular surgeon at Sentara Vascular Specialists in Norfolk, Virginia, declared: “The surgical challenges of repairing deep venous reflux have been present for more than a generation. It is worth reflecting on the fact that this new technology has made the majority of patients vastly better.” He was speaking as he presented podium-first efficacy results from the SAVVE trial.
“These patients are the most severe of the severe,” Dexter said. He described that the “vast majority—around 60%—of these patients have active ulcers.”












