An emerging program at Houston Methodist aims to help prod those practicing in the vascular surgical space deeper into the field of robotic surgery.
The first ah-ha during a talk at a national meeting being given by one of the foremost vascular surgeons in the U.S. The second came back at home base. The theme common to both? That major vascular operations and complications were being carried out by other specialties engaged in robotics-assisted surgery.
“I was at the Society for Clinical Vascular Surgery [SCVS] one year, and was watching a robotic left renal vein transposition—that’s a very sophisticated operation—by Sam Money, at that time the chief of the Mayo Clinic at Scottsdale,” says Alan Lumsden, MD, the Walter W. Fondren III Presidential Distinguished Chair at Houston Methodist’s DeBakey Heart & Vascular Center in Houston, Texas. “And then he said: ‘I didn’t do this operation, the urologist did it.’”

Then, back home in Houston, Lumsden was called to assist with a bleeding complication during a pelvic procedure being carried out by a gynecologist. When he arrived, the specialist—performing the procedure robotically—asked Lumsden if he could resolve some bleeding from an iliac artery using the robot. His response was in the negative. “I can’t do that,” he recalls saying. The gynecologist, unperturbed, then told him she would take care of the situation herself. “And I was dismissed,” he says. “Here is a major vascular operation being done by a urologist, and a major complication, that is normally in our bailiwick of repairing, now being done by the gynecologist.”
These experiences led to a realization—and a resolution. “We, in vascular surgery, have missed the boat on this,” says Lumsden. So he set about building a vascular robotics program.
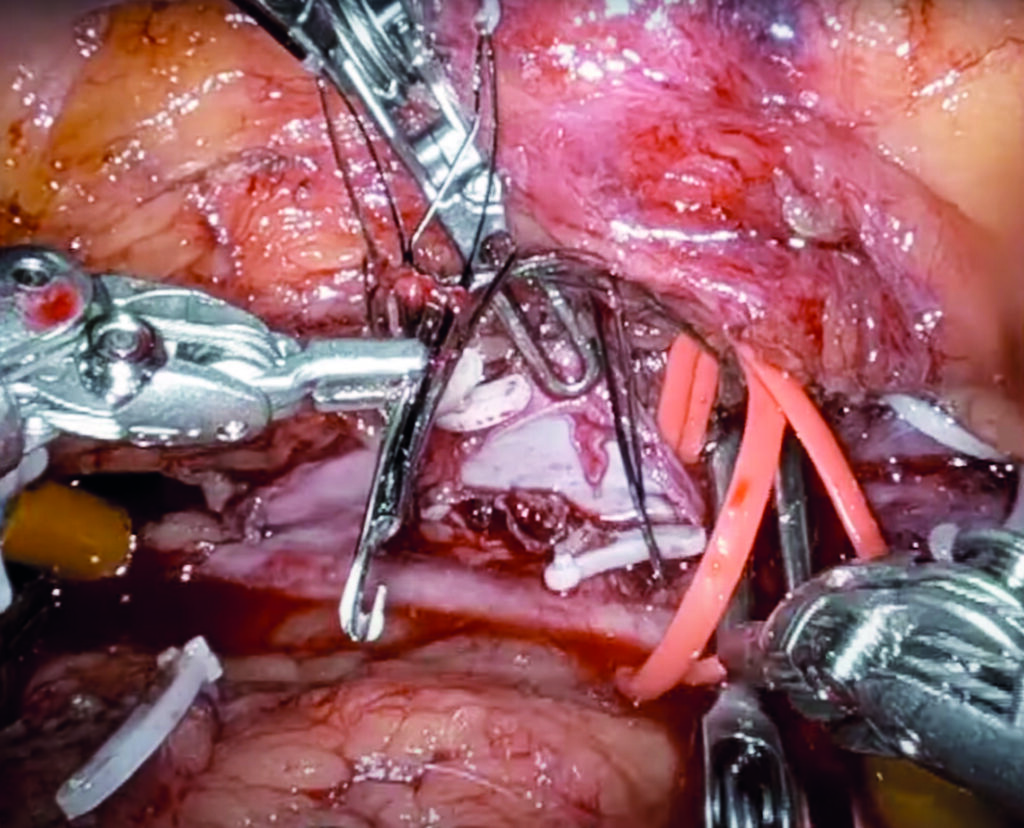
Of late, that program has been gaining some interested glances from around the country following dissemination of a video from the popular Houston Methodist DeBakey CV Education YouTube channel via social media. The video features an inferior vena cava (IVC) filter removal procedure performed robotically. The surgery was led by his colleague, Charudatta Bavare, MD, who in a DeBakey Heart & Vascular Center grand rounds from September 2022, proposed robotic vascular surgery as an “underexplored frontier,” raising the possibility that the open and endovascular era of the specialty may segue “into robotic vascular surgery in the future—that is the hope.”

Lumsden, who recently became president-elect of the Southern Association for Vascular Surgery (SAVS), stresses his role as “enabler” in this quest. For a long time, one of the challenges that held back vascular surgery was a lack of laparoscopic training, he points out. But these days, even many newer general surgeons “are now bypassing laparoscopic surgery and going straight to robotic,” he notes. “So this need for laparoscopic skills is not an absolute requirement to become a robotic surgeon.”
Lumsden sees his role as one of “pushing this along,” continuing: “You have got to learn the basics before you start taking on the big stuff. Charu[datta] Bavare is one of my mid-level partners, trained as a general surgeon, worked in the community in laparoscopic surgery, vascular surgery, general surgery—he had to go to what we call an underserved community—and he has got all the skills. If he can’t make this work, nobody can make it work.”
In Houston, Bavare started out on “relatively trivial cases,” explains Lumsden. Cases that perhaps do not require a robot, he says. “But you have to get up to speed in a safe environment. And you have to get your team up to speed.” From procedures such as laparoscopic peritoneal dialysis placement and revisions, Bavare moved on to the likes of median arcuate ligament syndrome, and, now, the IVC filter removal. “We have a lot of people here who are sophisticated in robotics, all of whom are interested in helping us do this,” Lumsden relates. “There are these little pieces we need in other specialties that we are actively trying to seek out and grab, and pull this toward the vascular surgery community.”
Lumsden looks back to the man for whom his center is named, Michael E. DeBakey, MD, and his innovation of the Dacron graft, as he looks forward. “To this day, that is probably the single-most durable procedure that has been described for repairing the aorta.” The problem with that was a “not-so-hot” delivery system, which the endovascular revolution sought to remedy. “What we’ve essentially done is given up durability for a delivery system. And that means stent grafts,” he says.
“If you look at other specialties—urology, general surgery—when they went minimally invasive, they went laparoscopic or robotic. They did the same procedures that have been proven for 20, 30 years. They didn’t invent a whole new specialty called endovascular surgery the way we bought into it.”












