This advertorial is sponsored by Surmodics.
Interventions for acute limb ischemia (ALI) represent up to 16% of the case volume for vascular surgeons and cost healthcare systems $26,000–$29,000 per patient in hospitalization costs.¹ While revascularization may be achieved via open or endovascular approaches, guidelines recommend selection of the technique that will provide the most rapid restoration of arterial flow with the least risk to the patient.²
Endovascular treatment to remove clots and restore blood flow is now a common alternative to surgery for revascularization in ALI.³ In recent years, percutaneous thrombectomy has become a viable option for vascular surgeons seeking single-session revascularization without the risks associated with thrombolytics4 or the need for costly intensive care unit (ICU) or hospital admissions.
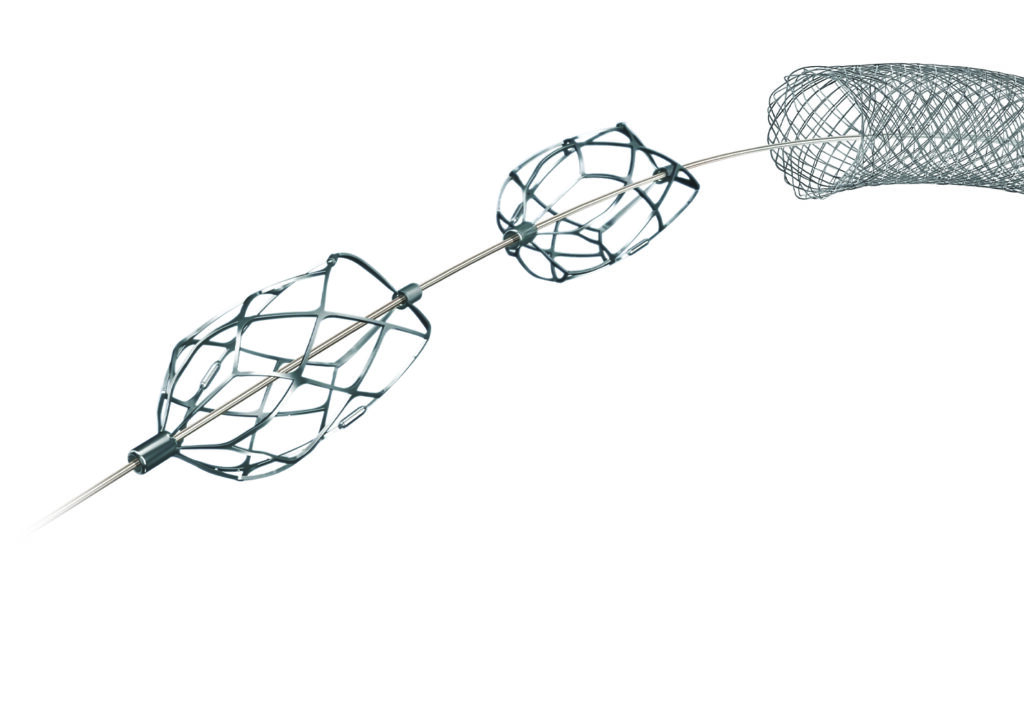
Until recently, the mainstays of percutaneous thrombectomy for ALI have been pharmacomechanical or aspiration devices. In 2021, Surmodics introduced the PounceTM Thrombectomy System, a purely mechanical solution that relies on a dual-basket technology to capture and remove chronic or acute emboli or thrombi without aspiration, lytics or capital equipment.
A 2023 retrospective study5 of 44 consecutive patients treated for lower extremity limb ischemia with suspected thrombus using the Pounce system demonstrated 83% technical success, defined in the study as effective removal of thrombus from the peripheral arterial segments where the system was used.
Notably, unlike previous studies of percutaneous thrombectomy devices in ALI, the study population included patients with subacute (15–30 days of symptoms; 16% of patients) and chronic (>30 days; 43% of patients) limb ischemia in addition to ALI (≤14 days; 41% of patients). In just one of 44 cases, thrombolysis was used to resolve thrombus secondary to treatment with the Pounce system. Procedural success, defined in the study as restoration of pulsatile flow to the foot and resolution of ischemic pain, was 95%.
Moving on from aspiration

Vascular surgeon Vince Weaver, MD (consultant to Surmodics), from the Vascular Specialty Center in Baton Rouge, Louisiana, uses percutaneous thrombectomy for most of his ALI cases. Today, the Pounce system is his go-to device.
“I’ve had access to just about all the arterial thrombectomy devices and have whittled them down,” he says. “Our practice still has the Angiojet pharmacomechanical system [Boston Scientific], but I really don’t use it anymore due to the use of tPA [tissue plasminogen activator] and [the] device’s systemic effects [e.g., renal impairment].”6
As for aspiration, Weaver used the Indigo aspiration system (Penumbra) and QuickClear thrombectomy system (Philips) as his primary percutaneous devices until about two years ago, when he started using the Pounce system. “The limitation I found with suction thrombectomy is that you could go in and take out a lot of fresh clot, but when you take your post-thrombectomy angiograms, you see that there’s a lot of residual thrombus and organized stuff remaining. With the Pounce system, after one, maybe two passes, I’ve been able to remove, if not all, at least a significant amount of that more organized thrombus. I’ve been getting much more robust thrombectomy with the device, and my success rate has been much higher for the right patient.”

Lucas Ferrer Cardona, MD (consultant to Surmodics), a vascular surgeon with the Dell Seton Medical Center at the University of Texas Hospital in Austin, has gravitated toward use of the Pounce system for similar reasons.
“The most significant benefit of the Pounce system over aspiration is that it’s effective in treating both acute and chronic clot,” he says. “Aspiration works great for fresh thrombus, but thrombus is usually not homogeneous.”
Efficiency and time management
Ferrer Cardona finds it efficient to be able to treat a range of heterogeneous clots with the PounceTM platform.
“For us, time management is critical. Elective procedures are 60% to 80% of our practice. We schedule these weeks in advance,” he says. “But patients with ALI or ALI and CLI [critical limb ischemia] can’t wait. They present at all times, and you have to treat them in a very time-sensitive manner because the outcomes are worse with delays. So, those two realities have to somehow coexist. That requires time management and efficiency.”
It takes him about 45 minutes to “treat what I’m going to treat with the Pounce system,” he says. “Let’s say I have an emergent patient come with rest pain; if, based on my experience, I feel confident I can get that patient in and out in a timely manner and bring in my other, scheduled patient— and my staff knows that and my cath lab manager knows that—then my flexibility to treat all patients and not have to put some things off and triage some patients increases significantly. Whatever makes that easier, more effective, and more predictable is going to benefit patients and the hospital. You’re using less human capital, you’re using less space, you’re using less time that can be used for treating additional patients.”
A new option for distal embolization
Vascular surgeons have also found significant benefit in using the Pounce platform as a bailout device for distal embolization during planned percutaneous lower-limb interventions. The PounceTM LP (Low-Profile ) Thrombectomy System, introduced in 2024, is intended for use in 2–4mm peripheral arteries, making it suitable for tibial occlusions. The original Pounce system is intended for use in 3.5–6mm arteries.

“Embolizing plaque is terrible, and we really have had limited options to get that embolus out,” says Christopher Leville, MD (consultant to Surmodics), a vascular surgeon with the CentraCare-St. Cloud Hospital in St. Cloud, Minnesota. “We used to try to use Export catheters [Medtronic] or other devices, or even a SpiderFX filter [Medtronic] or other devices, but everything was suboptimal. In these situations, you can use the Pounce LP system very quickly, without major setup. You just open the package, get out the embolus, and a major problem is often resolved within minutes without surgical cutdown or another procedure with tPA.”
Leville believes the Pounce platform’s mechanism of action is particularly suited for this application. “What I like about the Pounce platform is that it behaves more like a Fogarty balloon. You start distal to the thrombus and withdraw back, just as you would with a Fogarty. In situations where you’re concerned about distal embolization, it can make more sense to use a Pounce platform. We do Fogarty procedures without wire access all the time—you just thread the catheter down the leg, inflate the balloon, and withdraw the clot. The Pounce platform behaves very much like that. That’s why I use it. The last thing I want to do is to have to convert a case from percutaneous to open surgical or overnight tPA in the intensive care unit if that’s not what we had planned. The Pounce platform gives me a third option.”
References
- Gupta R, Siada SS, Bronsert M, Al-Musawi MH, Nehler MR, Jeniann AY. High rates of recurrent revascularization in acute limb ischemia–a national surgical quality improvement program study. Ann Vasc Surg. 2022;87:334–342
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;69(11):e71–126
- Lind B, Morcos O, Ferral H, et al. Endovascular strategies in the management of acute limb ischemia. Vasc Specialist Int. 2019;35(1):4
- Ebben HP, Jongkind V, Wisselink W, Hoksbergen AW, Yeung KK. Catheter directed thrombolysis protocols for peripheral arterial occlusions: a systematic review. Eur J Vasc Endovasc Surg. 2019;57(5):667–675
- Gray BH, Wheibe E, Dicks AB, Low ML, Tingen JS. Pounce thrombectomy system to treat acute and chronic peripheral arterial occlusions. Ann Vasc Surg. 2023;96:104-114
- Acosta S, Karonen E, Eek F, Butt T. Short-term complications and outcomes in Pharmaco-mechanical thrombolysis first and catheter-directed thrombolysis first in patients with acute lower limb ischemia. Ann Vasc Surg. 2023;94:253–262
Case reports
Removal of acute and organized SFA thrombus
 Vince Weaver highlights a case in which the thrombus in the left superficial femoral artery (SFA) is tackled.
Vince Weaver highlights a case in which the thrombus in the left superficial femoral artery (SFA) is tackled.
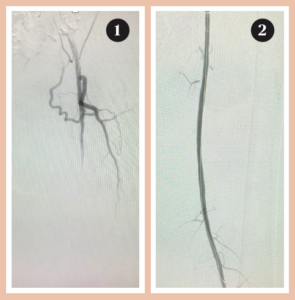
Patient presentation and diagnostics: A 45-year-old man with a history of embolic and thrombotic events presented with left leg pain of one-week duration. The initial angiogram (Figure 1) showed new arterial thrombus in the mid to distal left SFA.
Thrombectomy: The Pounce system basket wire was deployed distal to the thrombus and the funnel catheter deployed proximal to the thrombus. The baskets were withdrawn into the funnel catheter and the system was removed, completing the first device pass. Balloon angioplasty was also performed to clear residual disease. The final angiogram showed full restoration of SFA flow (Figure 2).
Post-procedure outcome: The patient was discharged the next day. The Pounce system aided in the removal of acute and organized thrombus in one pass.
Removal of organized infrapopliteal arterial thrombus
 Lucas Ferrer Cardona presents a case of complete thrombus in below-the-knee arteries.
Lucas Ferrer Cardona presents a case of complete thrombus in below-the-knee arteries.
Patient presentation and diagnostics: A male patient presented with immediate onset of numbness, pain and decreased function in his lower left leg. The initial angiogram showed complete thrombosis of the left popliteal, tibioperoneal trunk (TPT) and tibial arteries (Figure 1).
Thrombectomy: Two Pounce system passes removed organized thrombus from the popliteal artery, but distal flow continued to be hampered by an occlusion in the proximal anterior tibial (AT) artery. One pass with the Pounce LP System resulted in complete removal and resolution of the thrombus burden with improved flow through the AT to the plantar arch (Figure 2).
Post-procedure outcome: The patient was discharged after two days. The combination of Pounce and Pounce LP systems allowed for complete removal of organized thrombus from below-the-knee vessels without the need for thrombolytics or surgical intervention.
Removal of brachial and ulnar artery thrombus
 Christopher Leville demonstrates the use of Pounce LP in the upper extremity.
Christopher Leville demonstrates the use of Pounce LP in the upper extremity.
Patient presentation and diagnostics: A man in his late 60s presented with a cold left hand symptomatic for 24 hours. An initial ultrasound showed a partial occlusion of the left ulnar artery (Figure 1) and complete occlusion of the patient’s left brachial artery. The patient was not a candidate for tPA and open surgical thrombectomy was not deemed appropriate.
Thrombectomy: Two Pounce system passes in the mid and distal brachial artery, respectively, were followed by one Pounce LP system pass in the ulnar artery. Final angiograms showed complete resolution of the ulnar artery (Figure 2) and a patent brachial artery, with no embolization to the patient’s hand.
Post-procedure outcome: The patient was discharged the day after the intervention, with instructions to maintain his warfarin regimen for three months. At one-month follow-up, the patient’s brachial and ulnar arteries continued to show patency and good flow.
A version of this article first appeared in Endovascular Today.
Caution: Federal (U.S.) law restricts the Pounce™ Thrombectomy System and Pounce™ LP Thrombectomy System to sale by or on the order of a physician. Please refer to each product’s Instructions for Use for indications, contraindications, warnings and precautions. SURMODICS, POUNCE, and SURMODICS and POUNCE logos are trademarks of Surmodics, Inc., and/or its affiliates. Third-party trademarks are the property of their respective owners.











