A retrospective analysis published in the Journal of Vascular Access (JVA) has shown that the oversized balloon angioplasty technique to assist arteriovenous (AV) fistula maturation is safe and effective—and allows cannulation of the fistula within hours or days of the procedure, decreasing the time a central venous catheter (CVC) needs to be used for.
In their JVA report, lead author Leonardo de Oliveira Harduin, MD, a vascular and endovascular surgeon at LivCare Centro Clínico in Rio de Janeiro, Brazil, and colleagues write: “In the present study, the vast majority of AV fistulas unsuitable for cannulation eight weeks after its creation became a functional vascular access for hemodialysis following balloon angioplasty. In this series, technical and clinical success was achieved in 91% of cases. Previous studies have demonstrated comparable technical success, ranging from 74% to 97%, with use of an endovascular technique for AV fistula maturation based on balloon angioplasty.”
Despite the fact that the functional autologous AV fistula is considered the best vascular access for patients on hemodialysis, Harduin et al note, some fistulas exhibit maturation problems after creation, and do not reach adequate vessel diameter and flow in dialysis. As such, the researchers aimed to describe their technique of oversized balloon angioplasty for the assisted maturation of AV fistulas, as well as the safety and efficacy outcomes associated with it.
They conducted a single-centre, retrospective chart review on both the inpatient and outpatient records of patients who had undergone AV fistula creation, but whose fistula had failed to mature and was not fit for use in dialysis access eight weeks after the procedure, and later received endovascular therapy to assist fistula development.
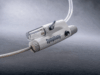
Patients underwent imaging procedures to identify stenosis, followed by angioplasty using oversized, high-pressure balloons from the anastomosis to the deep venous outflow tract. The veins were pre-dilated with balloons 5–7mm in diameter, followed by a final dilation with 8–10mm balloons. The choice of the final diameter of the balloon was based on the diameter of the vein found at the preoperative vascular ultrasound. In most procedures during the dilatations, a team member maintained a control of the inflow by compressing the anastomosis because, as Harduin et al assert, this maneuver decreases the chances of rupture during the procedure.

The flow volume, time interval of use of the fistula and removal of the catheter, patency rates, and complications rates, were all evaluated in the review. From October 2011 to January 2019, 78 patients (41 men) with a mean age of 62±15 years (range=24–91 years) underwent 124 balloon angioplasty procedures for assisted AV fistula maturation, Harduin and colleagues report. All patients were on long-term hemodialysis through a catheter.
The average flow volume in their fistulas before the procedure was 276ml/min (range=122–488ml/min), and the mean time between fistula creation and the first salvage procedure was 15 weeks. Angioplasty was performed via direct cannulation of the AV fistula in 60% of cases (n=47), through the femoral vein in 18% of cases (n=14), through the radial artery in 10% of cases (n=8) and by cannulation of the brachial artery in 4% of cases (n=3). In six patients (8%), double puncture of the AV fistula was needed to treat multiple existing stenoses, the authors also note.
Technical and clinical success was achieved in 91% of patients (n=71) across the review. Seven patients were excluded—two of these exclusions were due to complete rupture of the AV fistula requiring ligation and five were because of 50% residual stenosis, leading to maturation of the AV fistula being considered unfeasible—and a new access route for dialysis being established.
In patients with successful maturation, no residual stenoses were identified at angiography, the vein became palpable throughout the matured segment, the average flow volume was 1014ml/min (range=760–1800ml/min) 24 hours after the procedure, and there was a 4+/4+ thrill at the end of the procedure, Harduin et al state. The mean time to first AV fistula use after maturation was five days (range=1–20 days) and, on average, catheter removal was performed 14 days (range=5–33 days) after the maturation procedure. In the 71 patients who experienced technical and clinical success, the primary patency rate at three, six and 12 months was 87.3%, 66.2%, and 50.7%, respectively.
Across the 124 procedures performed, minor complications occurred in 22 patients (18%), and six patients had major complications (4.8%), including two with grade I dialysis access steal syndrome, treated clinically, and two with an expanding pseudoaneurysm and localized pain in the area of maturation, requiring placement of a covered stent. During follow-up, 24 patients required an additional procedure and 11 patients required two additional procedures for fistula maturation and patency maintenance, with the mean time between these revision procedures being 5.6 months.
Kaplan-Meier analysis of the subgroups based on gender, age, diabetes status, and AV fistula site, showed that female gender was the only variable associated with reduced primary patency following balloon-assisted maturation, as women had significantly lower 12-month primary patency rates when compared to men (32.4% vs 67.6%, p=0.003). The number of surgical interventions per patient was also significantly higher in women than in men (2.09±0.83 procedures vs 1.43±0.69 procedures).
In addition to concluding that the oversized balloon-assisted AV fistula maturation technique was shown to be safe and effective, the authors write that the 12-month patency rates obtained were “encouraging,” and equivalent to those described for AV fistulas that matured without intervention.
SOURCE: doi.org/10.1177/11297298211029558