For the public, navigating the complex world of vascular care must seem like being adrift on the high seas, with brigands and pirates galore. Vascular surgeons, cardiac surgeons, interventional radiologists, and interventional cardiologists all raise their friendly flags to lure patients. How about vascular medicine, interventional nephrology, and other specialties that sound like a Medical Mad Libs game gone bad? Where to go for care? What is a Heart and Vascular Center? And what about those freestanding labs? You can practically hear the sweet sound of unindicated atherectomies from the streets outside.
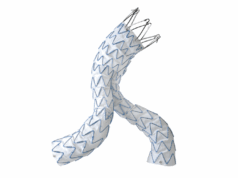
Renal stents, EVAR, SFA interventions, EVLT. The question is not who can do them, but who should? When I was a child, I assumed adults were smart. Adults must always have a plan. Now, faced with daily incontrovertible evidence to the contrary, I am ready to cede these points. There is no plan, but there should be.
In the mid-2000s, interventional cardiologists, faced with declining coronary interventions, expanded their interest in other vascular territories. Somehow, despite every metric showing a reduction in their case volume, interventional cardiologists grew their workforce in historic fashion. Between 2008 and 2013, the U.S. workforce of interventional cardiologists nearly doubled, the largest expansion of any medical or surgical specialty. Number two on the list? Interventional Radiology.
I believe the crux of this matter lies in the training of physicians. In the United States, the Accreditation Council for Graduate Medical Education (ACGME) sets standards and accredits residency and fellowship programs. Let us review their educational requirements and expectations for these programs with regard to peripheral vascular disease and treatment. First, throw out Vascular Medicine and Interventional Nephrology. The ACGME recognizes 150 specialties and subspecialties, but not these 2. Similarly, the American Board of Medical Specialties offers no certification in these self-designated fields.
Interventional cardiology, according to the ACGME, is “the practice of techniques that improve coronary circulation, alleviate valvular stenosis and regurgitation, and treat other structural heart disease.” Sounds good to me. Looking through the 33-page document that details the requirements for training in interventional cardiology, how often does the word carotid appear? Never. Venous? Zero. Aortic aneurysm? Nada. Any reference to peripheral vascular disease at all? Nope. Indeed the only requirement for knowledge of the peripheral vascular anatomy is in reference to percutaneous approaches to the heart. There is, however, a prerequisite for “application of evidence to patient care and advocacy for quality of care.” It seems the ACGME has my back here.
For other specialties, the training requirements have a tenuous, at best, relationship with vascular interventions. Thoracic Surgery trainees are required to have knowledge of abnormalities of the great vessels and thoracic aorta, but nothing beyond. Interventional radiology trainees must learn to perform “arterial and venous interventions;” but no specific vascular regions are given. Dermatologists need knowledge of vein therapies but neither performance of these procedures nor even direct observation are required.
What then of the trainee case logs? Evidence of their clinical experience? Trainees in interventional cardiology and interventional radiology are not required to use the ACGME case logs. Interventional cardiology fellows only use self-reported case logs and the sole requirement is 250 coronary interventions. In fact, of all the germane specialties, only vascular surgery requires detailed reporting with minimum requirements in multiple vascular trees. Vascular surgery is also the only relevant specialty to report the national averages of the graduates’ case volumes on the public ACGME website.
Education is a process; we acquire competence from the competent. The treatment of peripheral vascular disease is a vocation, not a hobby. “Interest” or even “experience” does not translate to aptitude and proficiency. Whatever one’s issues with the ACGME, they have laid out the most rigorous standards for medical training that exist. Vascular surgery is the only specialty requiring and documenting comprehensive vascular training in all six competencies mandated by the ACGME. Who will tell my trainees, after years of residency, that someone doing a series of unregulated extracurricular activities has had an “equivalent experience”?
Technical teaching without cognitive instruction often results in inappropriate application of treatments. Costs rise and quality falls. Repeated exposure to a technique without consequence or accountability is not training. My 5 year old likes to sit on my lap and steer the car around the parking lot but I do not recommend you let him take you to the airport. What-to-do takes longer to learn than how-to-do-it. In the early years after your training finished, when you called your mentor about a case, what did you ask? In most instances, the question was not how to technically perform a task, but rather what task to do.
The public’s trust in our training and motivation is implicit and necessary. But even doctors have difficulty determining the legitimacy of other specialties’ training in vascular pathology. To say nothing of the public or credentialing committees. Institutions like the ACGME should condemn physicians who chose to practice medicine that bears little resemblance to their intended training.
Peter Lawrence, MD, commenting on this issue in a letter to the New York Times (Feb. 12, 2015), wrote “Vascular Specialists need an in-depth understanding of vascular disease, as well as technical skill, but they also need the ethics to treat patients like a brother or sister, not the source of a payment for a new car.” Allowing so many practitioners to use unregulated pathways to gain credentialing in vascular interventions is folly. Vascular surgeons are the only specialists who have undergone comprehensive accredited training in the care of the vascular patient. We have more than seen it. We have more than done it. We have understood it.
Marriage, and 13 years working for a state institution, have taught me that it is far easier to change one’s own behavior than another’s. As a specialty, we share in the blame for this quagmire. We have been slow to grow our training programs thereby creating a shortage of vascular surgeons. Where we do not exist, others are happy to take up the slack. We cannot make the argument that these are our cases if we cannot cover them. Secondly, we have little public identity. Many medical students do not even understand the role of the vascular surgeon.
We have seemingly failed to brand ourselves to anyone but ourselves. The public must know who we are, where we are, and what we do. This is essential.
Dr. Sheahan is a professor of surgery and Program Director, Vascular Surgery Residency and Fellowship Programs, Louisiana State University Health Sciences Center, School of Medicine, New Orleans. He is also the Deputy Medical Editor of Vascular Specialist.