The Society for Vascular Surgery (SVS) and the American College of Surgeons (ACS) have launched the “Vascular Verification Program (Vascular-VP),” an ACS Quality Program developed in partnership with the SVS.
The newly launched inpatient program reviews not just safety processes against standards created by vascular surgeons, but also emphasizes the importance of using clinical data for tracking outcomes and supporting quality improvement specific to vascular care. It covers the perioperative continuum of care, from pre-hospital to post-discharge care.
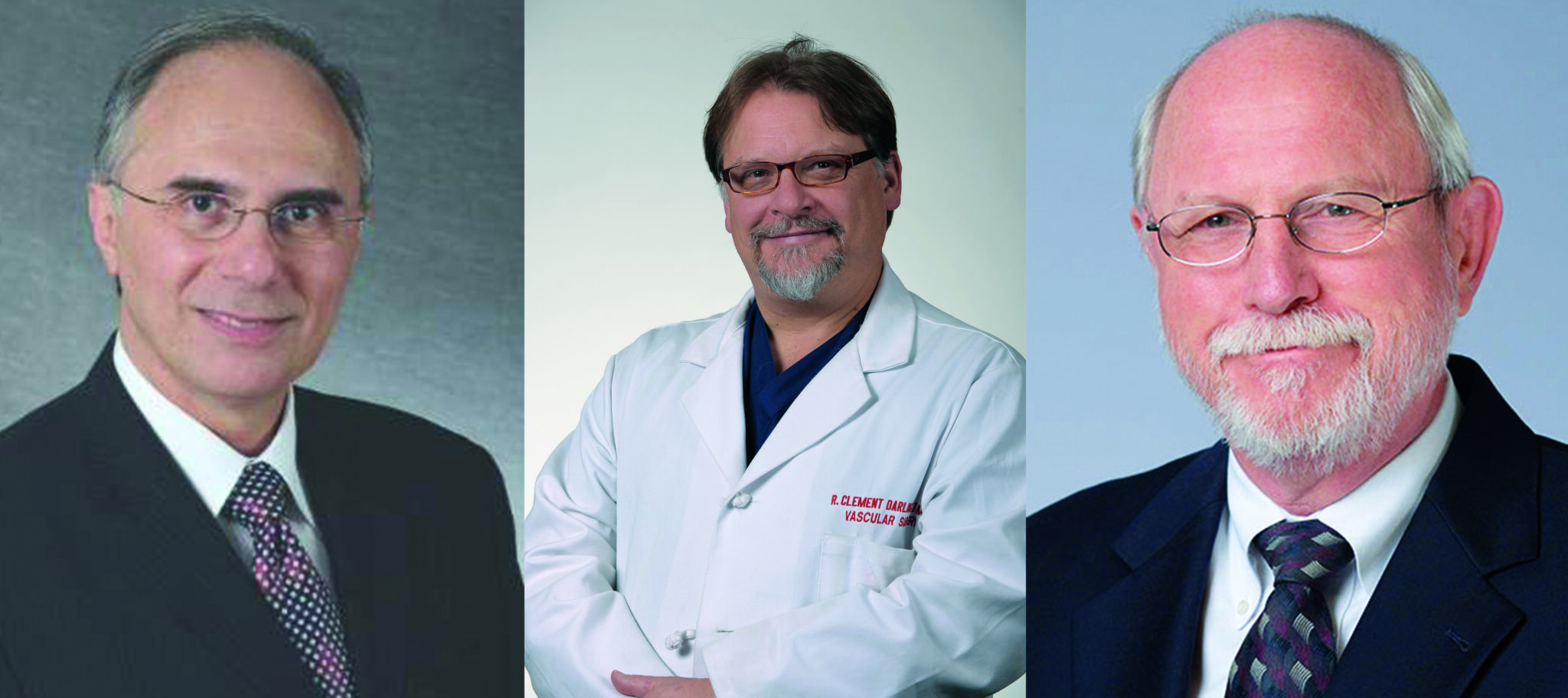
“We created this program to ensure quality and quality improvement in vascular care in both the inpatient and outpatient settings,” said SVS President Michael C. Dalsing, MD. “Our own members asked for this program, particularly for outpatient settings, which may have little or no oversight. They understand the importance of standard policies and procedures imbedded wherever care is provided to ensure safety and promote quality.”
The verification process ensures that an applicant program:
- Has the appropriate infrastructure for the procedures performed
- Follows clinical pathways to ensure care is in line with evidence-based clinical guidelines when available
- Monitors outcomes, emphasizing the importance of clinically relevant, risk-adjusted, nationally-benchmarked data
- Submits all needed information to reviewers who will assess all required aspects of the program for verification
- Undergoes a verification visit to ensure all standards are complied with and performs case review to ensure that there are internal quality processes in place to ensure safe and appropriate care of patients afflicted with vascular disease is provided
ACS has a long-standing experience in a wide array of quality verification programs to include cancer, trauma, bariatric surgery, pediatric surgery, to name a few. All these programs use the same structure used in the new Vascular-VP. This structure is based on four pillars:
- Standards based on peer-reviewed published data and expert consensus
- Appropriate infrastructure based on the standards designed for the program
- Data for monitoring outcomes and quality improvement support, using reliable, clinically relevant, benchmark data
- External peer-review team to verify compliance with the standards
“It was a win-win to work with the College for the vascular program,” said Anton Sidawy, MD, who, as the vascular regent serving on the Board of Regents of the ACS and past president of the SVS, led the effort to create the Vascular-VP. This is not the first time that the SVS sought such a program to ensure vascular centers are reviewed for quality.
“With the ongoing shift in reimbursement for our services from volume to value, who best to define quality and value than us—vascular surgeons and the professional organization representing us, the Society for Vascular Surgery?” Sidawy said.
Vascular diseases and issues covered in the program include, but are not limited to, thoracic-aortic, abdominal aortic, carotid artery disease, peripheral artery disease (PAD), arteriovenous hemodialysis access, and superficial and deep venous disease.
Those centers that meet the current inpatient standards will be “Verified” at one of two levels: a “comprehensive inpatient vascular center,” or “verified inpatient vascular center.”
Eight pilot programs—four inpatient and four outpatient—have already gone through the pilot phase of the verification process, including both the inpatient and outpatient components of Albany Medical Center in Albany, New York, under the direction of R. Clement Darling III, MD, chief of vascular surgery at the institution, and himself an SVS past president. He called the process “invaluable.” That includes ascertaining that Albany Medical “had the components we always thought we did. We found out we need to do better in some areas and actually begin implementing procedures in other areas.”
Administrators at Albany Medical Center found it eye-opening to see how much work goes into a successful vascular program, Darling said, including “how comprehensive the infrastructure needs to be to care for these incredibly complex patients. It showed them what infrastructure we need from the hospital to provide the best care for our patients.”
Going through the process “made us better and helped us take better care of our patients,” Darling said, and urged other vascular centers to undertake the verification process.
The process also ensures the longitudinal care for which vascular surgeons are known for providing. “Our care doesn’t end in the OR [operating room],” said Darling. “Every move has to be documented and evaluated; this process lets us follow our patients to make sure we’re providing the best care for them.”
“As the program launches, more institutions are waiting in the wings, including my own in Indianapolis, Indiana,” added Dalsing.
He believes the new initiative will provide several benefits, including improvement in quality of care for patients, enhanced learning throughout the institution, and external credibility to regulators. “We set the standards and we’re reviewing the data,” said Dalsing. “This will help everyone understand that ‘quality vascular care’ should be the goal of every center that takes care of patients with vascular disease, and that this program is the tool to help us realize this goal.”
Sidawy, Darling and Dalsing all emphasized advantages for not only patient care but also potential improvements to vascular programs.
Those involved examine the entire process, such as: “What other support staff do we need? How can we maximize utilization of all the components in the system—not as just a vascular unit but also a vascular system that has significant impact on other specialties, such as orthopedics, oncology, spine, and cardiology?” Darling said. “We are an integral horizontal component for many high-end specialties. This process really documents the importance and impact of a vascular surgery system on the hospital system.”
As the program continues, those who already have gone through the process will be able to share information and experiences with other vascular surgeons embarking on verification. “Much of the information we used in putting together our data could be shared as to what protocols were important,” Darling said. “This gives us a consistency and accountability across the country for expert vascular care.”
Dalsing, Darling, and Sidawy stressed that quality and quality improvement are at the heart of the Vascular-VP, the only program available that establishes and verifies a programmatic approach to quality in vascular care.
In the end it comes down to ensuring quality, said Dalsing. “SVS is all about quality. It is our North Star.”
Facilities involved in pilot site visits
Pilot sites involved in the verification program were, for inpatient: Albany Medical Center; Baylor Scott & White Heart Hospital in Plano, Texas; the University of California, San Francisco Vascular Program; and Keck Hospital of University of Southern California.
Outpatient sites were Albany Medical Center; Michigan Vascular Center; Nashville Vascular and Vein Center in Tennessee; and Vascular Institute of New York/Total Vascular Center in Brooklyn, New York.
SVS members involved in the pilot site visits are, respectively, R. Clement Darling III, MD, William Shutze, MD, Michael Conte, MD, and Fred Weaver, MD, for inpatient facilities and Darling, Robert Molnar, MD, Patrick Ryan, MD, and Anil Hingorani, MD, for outpatient facilities.