The speed with which artificial intelligence (AI) is beginning to envelope aspects of the human experience strikes many as jarring. Its entrance into the world of vascular surgery, too, has picked up a pace in recent years, with models and applications beginning to pop up in papers probing aspects of AI uses in care across the vasculature. But what is the extent of its abilities in vascular practice and where might AI lead the field in the future?
The speed with which artificial intelligence (AI) is beginning to envelope aspects of the human experience strikes many as jarring. Its entrance into the world of vascular surgery, too, has picked up a pace in recent years, with models and applications beginning to pop up in papers probing aspects of AI uses in care across the vasculature. But what is the extent of its abilities in vascular practice and where might AI lead the field in the future?
There are challenges. But there are also opportunities. That was the argument from Amun G. Hofmann, MD, of Klinik Ottakring in Vienna, Austria, when he spoke about integrating AI in vascular surgery in a recent letter to the editor of the European Journal of Vascular and Endovascular Surgery (EJVES).
In another letter, this time to the editor of the Journal of Vascular Surgery (JVS) entitled “Artificial intelligence and legal implications,” Antonio V. Sterpetti, MD, and colleagues from Sapienza University in Rome, Italy, wrote that, “Recommendations made by AI should remain simple suggestions, which cannot substitute for the opinion of surgeons in a complex clinical analysis, to prevent legal controversies and to preserve the dignity of patients and vascular surgeons.”
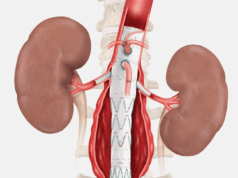
Sterpetti and colleagues were responding to a study by Joachim S. Skovbo, MD, of Odense University Hospital in Odense, Denmark, and colleagues, who in JVS had previously outlined the successful development of the SHAPFire AI tool to identify abdominal aortic aneurysms (AAAs) at increased risk of rupture with “significantly higher” accuracy than diameter alone.
AI papers are now myriad. At the 2025 Vascular Annual Meeting (VAM) in New Orleans earlier this summer, a full half of a plenary session was dedicated to emerging AI uses in vascular surgery. At the Eastern Vascular Society (EVS) annual meeting in Nashville, Tennessee, next month, data scientist Yelena Yesha, PhD, is set to speak on the “brave new world” of AI and data science in the field.
So what does that brave new world look like right now?
One of the papers at VAM 2025 looked at the use of a large language model—in common parlance the ChatGPTs of the world—to accurately extract aortic information from abdominal imaging reports in a large, real-world, multicenter database in San Francisco, California. Robert Chang, MD, assistant chair of vascular surgery at Kaiser Permanente Northern California, and Colleen Flanagan, MD, chief resident in the UCSF Division of Vascular and Endovascular Surgery, who led the study, found that an open source or “off-the-shelf ” large language model was able to extract critical information about the aorta from 16,000 AAA imaging reports from across 16 years. This “was consistent” across multiple imaging modalities, they noted. “The accuracy of the model, LLaMa 3.3, was over 90% overall and across a number of these subcategories,” Chang and Flanagan told Vascular Specialist. “We think this could support our ability to closely track AAAs.”
The same VAM 2025 session saw Justin Bader, MD, present a paper outlining the creation of a prediction model for safe contrast volume thresholds to prevent post-contrast acute kidney injury (PC-AKI) after endovascular aneurysm repair (EVAR). The research team is now using AI to harness the model’s future potential. Bader, a general surgery resident at Yale School of Medicine in New Haven, Connecticut, explains that the team used data from 49,417 patients in the Vascular Quality Initiative (VQI) database to create a “calculator” that allows physicians to generate a recommended contrast volume to minimize PC-AKI risk by inputting 13 patient-specific variables. “It serves as a guideline for surgeons when they’re operating,” he says. The research team—led by Cassius Iyad Ochoa Chaar, MD, associate professor of surgery at Yale School of Medicine—reported that the model is “working extremely well,” Bader tells Vascular Specialist. The team is presently collaborating with statistics experts at Yale on advanced AI and machine learning techniques to get to “higher order relationships between variables to make it an even more accurate calculator.”
Ben Li, MD, a resident in the Division of Vascular Surgery at the University of Toronto, Canada, and colleagues had two AI papers at VAM 2025, one in the plenary session, the other a poster. The plenary paper looked at developing an AI model to predict one-year mortality after major lower extremity amputation, the poster to predict one-year successful clinical use of an arteriovenous access for hemodialysis. Using the VQI for both, they found that in both cases their machine learning models could “very accurately predict” outcomes and performed better than logistic regression. Li has tracked the development of AI uses in vascular surgery over the years in a review and found that though the number of papers on the topic has been increasing and the quality improving over the years, they remain “suboptimal.” A few AI applications are starting to be routinely implemented into clinical practice, Li observes, but stresses the importance of “developing the models in a robust way that follow guidelines.”
Meanwhile, the VAM session also saw data from Prem Chand Gupta, MD, head of vascular surgery at CARE Hospitals in Hyderabad, India, and colleagues that looked at the correlation of imaging characteristics of carotid plaque with clinical and histopathological features, and the application of AI. “We found that routinely performed ultrasound by us was better than CT [computed tomography] angiography and MR [magnetic resonance] angiography in deciding whether the plaque was vulnerable or not,” he tells Vascular Specialist. “Since ultrasound is very subjective, we applied AI to make the study more objective. So far, we have found the machine learning can recognize the carotid artery, and if there is a more than 50% narrowing, there is 96% chance it picks up that narrowing. We still have a long way to go because the machine learning will still require a lot more images.”
So where is AI in vascular surgery headed? Chang and Flanagan cite programs such as that highlighted in their use case: streamlining the running of an AAA surveillance program. “Other areas potentially include understanding the basis of vascular disease such as computer vision to assess aneurysm or plaque characteristics, cell and molecular modeling for drug discovery, and more advanced predictive analytics to help inform operative risk,” they say.
For Gupta, the idea that “not only could AI replace the diagnostics” but that it could be combined with robotics and “actually replace surgery too” is impossible to predict from the vantage point of today. “As of now, what we know is, even when we look at current evidence based on which we try to treat patients, there is always a physician modifier. I may not go by the evidence because my gut tells me, which AI is not going to be able to pick up. Similarly for surgery, there are just too many variables which come into surgery too. It is going to be very difficult for AI to have enough data to deal with different variables unless there is a human to guide it.”