Today’s Plenary Session 4—Hosted in Great Hall A, First Floor from 10:45 a.m.–12 p.m.—will feature a presentation of five-year findings from the VQI-VISION database indicating that aortobifemoral bypass (ABF) remains a more durable long-term treatment option compared to endovascular intervention for aortoiliac occlusive disease.
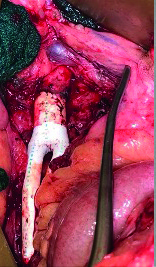
Elonay Yehualashet, BA, a medical student at Georgetown School of Medicine in Washington, D.C., is presenting these findings, which are also being discussed by senior author Natalie Sridharan, MD, assistant professor of surgery at the University of Pittsburgh Medical Center (UPMC) in Pittsburgh, Pennsylvania. “In medically appropriate patients, ABF may be beneficial and should be considered given its long-term results,” Yehualashet told VS@VAM.
For the present analysis, researchers queried the Vascular Quality Initiative (VQI) database for de novo aortoiliac interventions—ABF or supra-inguinal peripheral endovascular intervention (PVI)—and linked them to Medicare claims from 2010– 2019. Emergent cases and interventions for aneurysm or dissection were excluded.
The researchers’ primary endpoint was five-year estimates of freedom from major adverse limb events (MALE; major amputation or reintervention) or death, while a notable secondary endpoint consisted of freedom from major amputation or death. Kaplan-Meier analysis compared outcomes between patients undergoing ABF versus PVI and, additionally, subgroup analyses compared patients presenting with chronic limb-threatening ischemia (CLTI) versus claudication.
A total of 4,282 cases were identified—931 of which were ABFs (21.7%), 3,351 PVIs (78.2%). Over the study period, there was a trend toward increased PVI utilization, including 32.2% from 2010–2014 and 67.8% from 2015–2019 (p=0.01). Patients undergoing PVI were more likely to be older, live in urban areas and have higher rates of cardiovascular comorbidities, and had a greater likelihood of presenting with claudication, the researchers found.
As per their primary endpoint, the five-year rate of freedom from MALE or death was 58.7% in the ABF group and 38.2% in the PVI group (p<0.0001). Sequential Cox regression analysis demonstrated that the observed difference in the MALE/death rate between groups favoring ABF “persisted and remained significant” after adjustment for covariates of known clinical significance (adjusted hazard ratio [aHR] for PVI, 1.889; 95% confidence interval [CI], 1.648–2.166; p<0.0001)—a trend that remained true for patients undergoing treatment for both claudication (aHR, 1.807; 95% CI, 1.498–2.18; p<0.001) and CLTI (aHR, 1.959; 95% CI, 1.605–2.392; p<0.0001).
Freedom from major amputation or death at five years was 70.5% in the ABF group and 60.1% in the PVI group (p<0.0001), and—as per subgroup analyses—PVI was only associated with increased risks of major amputation or death among CLTI patients (aHR, 1.665; 95% CI, 1.311–2.114; p<0.0001), but not among those with claudication. The researchers speculate based on this finding that more prevalent MALE in patients undergoing PVI for claudication is related specifically to increased numbers of reinterventions.
“Despite the shift toward an endovascular-first approach for aortoiliac occlusive disease, the durability of suprainguinal PVI may not persist long-term,” Yehualashet and colleagues conclude. “In medically appropriate patients, ABF may offer CLTI patients improved limb preservation, while patients with claudication may experience reduced reintervention rates.”












