At this year’s International Symposium on Endovascular Therapy (ISET), being held Jan. 16–19 in Hollywood, Florida, experts presented an array of late-breaking trial results on topics ranging from venous stenting to abdominal aortic aneurysm (AAA) sac sealing.
Waseem Wahood, MS, a medical student at Dr. Kiran C Patel College of Allopathic Medicine in Davie, Florida, gave a U.S. national perspective on disparities in the treatment of peripheral arterial disease (PAD) and chronic limb-threatening ischemia (CLTI). The presenter highlighted major disparities in PAD and CLTI treatments for non-white populations, detailing that non-white patients are more likely to receive amputations, and less likely to receive revascularization (for PAD) compared to white patients. However, Wahood stressed that “the gap is slowly closing,” which “may demonstrate that guidelines have been effective in mitigating disparities.”
George Adams, MD, UNC REX Healthcare, Chapel Hill, North Carolina, delivered the results of a pooled subanalysis from the Tack optimized balloon angioplasty (TOBA) studies of the Tack endovascular system (Intact Vascular/Philips). The TOBA studies are unique, he informed the ISET audience, in that they are the first and only studies to enroll 100% dissected arteries. The studies demonstrate very low rates of clinically-driven target lesion revascularization (CD-TLR) and bailout stenting, he summarized, concluding that dissection repair with Tack produces positive short- and long-term results while preserving future treatment options.
Relaying findings from a multicenter experience with the WavelinQ endovascular arteriovenous fistula (endoAVF) 4Fr system (BD), Bulent Arslan, MD, of Rush University Medical Center in Chicago detailed a 72% primary patency, 88% secondary patency, 78% successful two-needle cannulation and 80.7% freedom from reintervention in 120 patients—the largest series to date, he claimed. Arslan encouraged attendees to look out for the results of ongoing clinical trials in the space, including WAVE-Global and CONNECT-AV, both designed to assess WavelinQ, and also the Ellipsys vascular access system (Avenu Medical/Medtronic) postmarket surveillance study.
Also on the agenda were the latest data on venous stenting. Erin Murphy, MD, director of Venous and Lymphatic Institute at Sanger Heart and Vascular, Atrium Health, Charlotte, North Carolina, outlined 24-month data from the ABRE trial—a prospective, multicenter, single-arm study of 200 patients with symptomatic iliofemoral venous outflow treated with the Abre venous self-expanding stent system (Medtronic).
The presenter revealed that effectiveness was sustained though 24 months, with a primary patency of 85.7% and freedom from CD-TLR of 90.9%. In addition, Murphy communicated that no stent fractures and no stent migrations were reported through 24 months. Finally, the presenter detailed that all patients demonstrated sustained and clinically meaningful improvements in quality of life measures and venous functional assessment scored at 24 months.
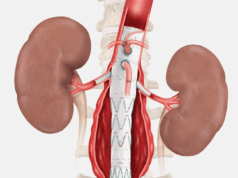
In the abdominal aortic space, Andrew Holden, MBChB, of Auckland Hospital, Auckland, New Zealand) spoke on AAA sac sealing with the Impede-FX RapidFill embolisation plug (Shape Memory). He conveyed early data from the AAA-SHAPE early feasibility studies—prospective, multicenter investigations being conducted at two centers in New Zealand and three in The Netherlands. In the period September 2020–December 2021, 16 patients were treated for endovascular aneurysm repair (EVAR), Holden detailed, reporting a 100% technical success rate so far and concluding that AAA sac filling during EVAR with Impede-FX RapidFill may improve aneurysm sac regression and reduce endoleak. However, he stressed that these are preliminary data from an ongoing investigation and that continued studies with long-term follow-up are needed.
Finally, Ripal Gandhi, MD, of Miami Cardiac & Vascular Institute and Miami Cancer Institute, Miami, expanded on an interim analysis of the RESCUE trial presented by Akhilesh Sista, MD, of New York University School of Medicine, New York, at Vascular Interventional Advances (VIVA) 2021 (Oct. 5–7) in Las Vegas. The RESCUE trial is a multicenter, prospective single-arm clinical trial, which is evaluating the safety and efficacy of pharmacomechanical catheter-directed thrombolysis with the Bashir endovascular catheter, specifically in patients with intermediate-risk acute pulmonary embolism.
The interim analysis included 62 patients and showed a reduction in the right ventricular to left ventricular (RV/LV) ratio of 32.1%, at 48 hours. There was also a reduction in the thrombus burden, as measured by the Modified Miller index on the computed tomography (CT) scan of 36.3%, at 48 hours and no major bleeding or device-related adverse events.
“The new datapoints are that there was a 90% reduction in the number of totally occluded segmental pulmonary arteries, and a 72% reduction in the total, or subtotal occlusions by 48 hours, as measured on a CT angiogram. This is really remarkable, because when we look at this reduction, this treatment is quite striking, and has never been reported with any other treatment modality that we have seen yet for pulmonary embolism. In fact, the mean number of occluded segmental arteries per patient that decreased by 72.5%. The restoration of the pulmonary arterial blood flow, really should be an important goal for treatment, and has not really been evaluated well in other studies for acute pulmonary embolism to date,” Gandhi exclusively told Vascular News, a Vascular Specialist partner title.