In a recently published study, dedicated venous stents performed well through pregnancy and postpartum, and a protocol including the use of low-dose antiplatelets in combination with anticoagulation at either a prophylactic or therapeutic dose depending on the patient’s risk profile appeared safe and effective.
In a recently published study, dedicated venous stents performed well through pregnancy and postpartum, and a protocol including the use of low-dose antiplatelets in combination with anticoagulation at either a prophylactic or therapeutic dose depending on the patient’s risk profile appeared safe and effective.
Writing in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (JVS-VL), authors Laurencia Villalba (Vascular Care Centre, Wollongong, Australia) and Theresa A Larkin (University of Wollongong, Wollongong, Australia) share that the aim of their study was to assess the performance of dedicated iliac venous stents during subsequent pregnancy and postpartum, including stent patency and stent integrity, as well as incidence of venous thromboembolism (VTE) and bleeding complications.
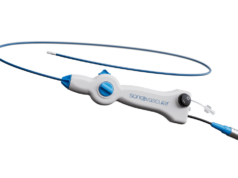
The investigators outline in their introduction that, while venous stenting has become the preferred method of treatment for non-thrombotic iliac vein lesions, post-thrombotic lesions, and lesions found after thrombus removal in the setting of an acute iliofemoral deep vein thrombosis, “concern remains about stenting women of child-bearing age”. They explain that this is because pregnancy is a hypercoagulable state, and the gravid uterus can potentially compress the stent and/or the inflow vessels and thus compromise patency. Villalba and Larkin add that the current literature on the performance of venous stentings during pregnancy comprises only six studies to date, including 66 patients and 74 pregnancies with most stents assessed being Wallstents (Boston Scientific).
This was a single-site, prospective cohort study. Villalba and Larkin detail that women of child-bearing age who had received dedicated iliac venous stents were included in a surveillance program and then, for any subsequent pregnancies, followed the same pregnancy care protocol. They explain that this included an antithrombotic regimen of 100mg aspirin daily until gestation week 36, and subcutaneous enoxaparin at a dose dependent on risk of thrombosis. Going into more detail, Villalba and Larkin specify that low-risk patients, those stented for non-thrombotic iliac vein lesions, received a prophylactic dose of 40mg/day from the third trimester, while high-risk patients, those stented for thrombotic indication, received a therapeutic dose of 1.5mg/kg/day from the first trimester. All women underwent follow-up with duplex ultrasound assessment of stent patency during pregnancy and six weeks postpartum, the authors note.
The authors report that, among 10 women who had received dedicated iliac venous stents for either a non-thrombotic or thrombotic indication, and 13 post-stent pregnancies—during which a dedicated protocol for stent thrombosis prevention was followed—there was a 100% patency rate, no bleeding complications, and no VTE during pregnancy or puerperium. Only one stent was permanently deformed /compressed by the gravid uterus, but it was a Vici stent that had been “balloon fenestrated” at the time of insertion due to concerns of contralateral caging, so it had lost its structural integrity.
In the discussion of their findings, the investigators write that the main limitation of their study is its small sample size. In addition, they acknowledge that it is still unknown whether multiple pregnancies could affect stent structure over time, despite three patients having two pregnancies each.
Villalba and Larkin also highlight the study’s key strengths, including the fact that patients were followed up prospectively, and that the investigators followed a protocol including serial imaging, multidisciplinary input and a tailored antithrombotic regime.
“Dedicated iliac venous stents perform well during subsequent pregnancy with no stent occlusion or fracture,” Villalba and Larkin conclude. They state in closing that child-bearing age “should not be a contraindication to venous stenting,” though they also stress that studies reporting on a larger sample size of patients are necessary.