Findings from a series of late-breaking trials in the endovascular field were delivered recently at TCT Connect (Oct. 14–18), the 32nd annual scientific symposium of the Cardiovascular Research Foundation (CRF), held virtually, with the first from Connie N. Hess, MD, of the University of Colorado in Aurora, featuring the results from a large subgroup analysis of the VOYAGER PAD randomized clinical trial.
The study showed neither a mortality risk nor benefit associated with the use of paclitaxel drug-coated devices in the treatment of peripheral arterial disease (PAD). The study also found that the benefit of rivaroxaban use on reducing ischemic limb and cardiovascular outcomes was consistent regardless of whether a drug-coated device was used.
Hess and team’s analysis examined the long-term safety of drug-coated devices (DCDs). It also evaluated whether rivaroxaban 2.5mg twice daily plus low dose aspirin versus low dose aspirin alone was consistent, either with or without use of a DCD.
During the qualifying endovascular lower extremity revascularization, DCD was used for 31% (n=1,358) of patients. Patients receiving DCD more frequently had prior endovascular lower extremity revascularization, had higher baseline use of dual antiplatelet therapy and statins, and were more often treated for claudication than non-DCD patients.
In the unweighted analysis, lower associated mortality was observed among patients receiving DCD versus non-DCD (2.9 vs. 3.9 per 100 patient-years; 3.5-year Kaplan-Meier cumulative incidence of 10.2% vs.13.8%). After weighting, there was no association between DCD use and mortality (3.5-year cumulative incidence 12.1% vs. 12.6%, HR 0.95, 95% CI 0.83-1.09, p=0.49). The benefit of rivaroxaban 2.5mg twice daily with aspirin compared to aspirin alone on reducing ischemic limb and cardiovascular outcomes was also consistent regardless of whether a DCD was used.
The VOYAGER PAD trial was funded by research grants to CPC Clinical Research from Bayer and Janssen.
IN.PACT 0.014 DCB may offer a clinical benefit in patients with CLI
Antonio Micari, MD, University of Messina, Messina, Italy, presented first-ever results from Medtronic’s IN.PACT BTK study, a feasibility study assessing the safety and effectiveness of the company’s IN.PACT 0.014 drug-coated balloon (DCB) in critical limb ischemia (CLI) patients with chronic total occlusion (CTO) in the infrapopliteal arteries.
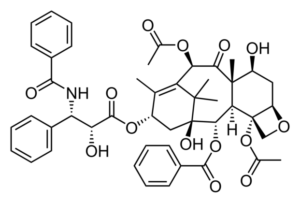
The IN.PACT BTK study is a prospective, multicenter, 1:1, randomized feasibility study assessing the safety and effectiveness of the IN.PACT 0.014 DCB, a 3.5 μg/mm2 dose paclitaxel-coated balloon, versus conventional percutaneous transluminal angioplasty (PTA) for the treatment of CTOs in the infrapopliteal arteries. The study enrolled 50 patients at nine sites in Europe.
At nine months, patients in the DCB group experienced a reduction in sub-segmental late lumen loss compared to those in the PTA control group (0.59±0.94mm versus 1.26±0.81mm, respectively, p=0.017), a 53% lower late lumen loss than the PTA control group. Using the classic late lumen loss method, subjects in the DCB group experienced lower late lumen loss compared to those in the PTA control group at nine months (0.89±0.77mm versus 1.31±0.72mm respectively, p=0.07 ), a 32% lower late lumen loss than the PTA control group.
Historically, there has not been a DCB technology that has demonstrated effectiveness in this vessel bed. According to a Medtronic press release, the data presented at TCT demonstrate that IN.PACT 0.014 may offer a clinical benefit in patients with CLI.
The IN.PACT 0.014 DCB is an investigational device that is being evaluated in Europe, and is not currently being evaluated in the U.S.
ILLUMENATE Global: Four-year results support durable long-term outcomes with the Stellarex DCB
Andrew Holden, MBChB, of Auckland City Hospital, Auckland, New Zealand, reported on late safety and efficacy outcomes for the low-dose Stellarex DCB (Philips) in de novo and restenotic femoropopliteal lesions from a large cohort.
He revealed that four-year data from the trial show favorable safety and efficacy outcomes consistent with the ILLUMENATE randomized controlled trials, and also demonstrate similar efficacy in prespecified cohorts including different gender groups and diabetics.
ILLUMENATE Global is a prospective, single-arm, multicenter study conducted in the EU. The patient population included those with Rutherford Clinical Classification (RCC) of 2–4 indicated for treatment of the superficial femoral artery (SFA) and/or popliteal artery for de novo or restenotic lesions. Follow-up office visits were at one, six, 12, 24, and 36-months post-procedure and included clinical, hemodynamic, and functional outcomes.
At four years, the rate of major target limb amputation was 0.8% and that of all-cause mortality was 8.1%. Clinically-driven target lesion revascularization through four years was 75.6% at day 1,460 and the subgroup analysis revealed no difference in prespecified cohorts.
“The ILLUMENATE Global study supports durable long-term outcomes with the Stellarex DCB and is applicable to a complex population,” Holden told the TCT audience.
Paclitaxel controversy
“I think we are really starting to close the door on the paclitaxel controversy,” Robert A. Lookstein, MD, of Mount Sinai Health System in New York, part of the panel for the TCT late-breaking trials, commented at the end of the session. “There is clearly a lot more work that needs to be done for paclitaxel below the knee and it is encouraging to see that there is going to be work on that,” he added. “We are barely scratching the surface on drug-based delivery in the below-knee circulation, so there is a lot more work to do.”












