 The Society for Vascular Surgery (SVS) has submitted comment letters in response to the proposed rules issued by the Centers for Medicare and Medicaid Services (CMS) on Medicare Physician Fee Schedule (MPFS) and the Medicare Hospital Outpatient Perspective Payment System and Ambulatory Surgical Center Payment System (OPPS). Both proposed rules are for calendar year (CY) 2023.
The Society for Vascular Surgery (SVS) has submitted comment letters in response to the proposed rules issued by the Centers for Medicare and Medicaid Services (CMS) on Medicare Physician Fee Schedule (MPFS) and the Medicare Hospital Outpatient Perspective Payment System and Ambulatory Surgical Center Payment System (OPPS). Both proposed rules are for calendar year (CY) 2023.
Each year CMS announces proposed rules for the MPFS and the OPPS, usually in July, and provides a 60-day comment period when the public can submit input on the proposed rules. After reviewing the comments, CMS issues final rules on the MPFS and OPPS, typically on or around Nov. 1; rules take effect on Jan. 1 of the following calendar year.
Members of the SVS Coding and Performance and Measures committees review these rules each year and assist in developing the SVS comment letters submitted to CMS. This year’s MPFS and OPPS proposed rules contained several important issues that impact vascular surgeons.
MPFS rule comment letter
In the comments on CY 2023 MPFS proposed rule, SVS members stressed the need for stability in Medicare physician payment. The CMS proposes to reduce the MPFS conversion factor by nearly 4.5%, rebase and revise the Medicare Economic Index (MEI) and move forward with year two of the four-year implementation of the clinical labor pricing update finalized in the CY 2022 MPFS rule. This will result in payment cuts that are unsustainable for vascular surgeons.
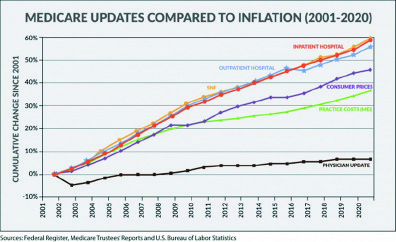
This recurring scenario with the annual MPFS payment rule that necessitates congressional action to mitigate Medicare payment cuts demonstrates that the Medicare physician payment system is broken. Factors that adversely impact the physician payment system are the lack of an annual inflationary update and the statutory budget-neutrality requirements that trigger across-the-board decreases in payment for all physicians when increases are provided for any physician fee schedule service. Updates to the conversion factor have consistently failed to keep up with inflation, in large part due to the fee schedule budget-neutrality requirements as depicted in the chart below. We strongly stated to CMS that “our policy-makers, both within the Administration and in Congress, have a duty to ensure a Medicare system that provides financial stability through a baseline positive annual update reflecting inflation in practice costs, and eliminate, replace or revise budget-neutrality requirements to allow for appropriate changes in spending growth.”
Percutaneous arteriovenous fistula creation
We requested that CMS reconsider its rejection of the RUC recommended work Relative Value Units of 7.50 for CPT code 368X1 and 9.60 for 368X2. The CMS proposed work RVUs of 7.20 for CPT code 368X1 and 9.30 for CPT code 368X2 do not accurately reflect the intensity of the physician work associated with these services. We believe the RVS Update Committee (RUC)-recommended values for these codes account for the complexity and intensity of the procedures and are supported through the survey data collected. We urged CMS to accept the RUC-recommended work RVUs of 7.50 for CPT code 368X1 and 9.60 for CPT code 368X2.
SVS commended CMS for accepting the RUC-recommended increased work values for the hospital inpatient and observation codes. However, we reiterated our strong objection to CMS’ continued refusal to incorporate the 2021 office Evaluation and Management (E/M) visit increases to the visits bundled into global surgery payment.
CMS requested public comment on strategies to improve the accuracy of payment for the global surgical packages. We expressed strong opposition to the CMS position that physicians are not performing the follow-up care with their patients that is included in the global surgical package. Noting the many flaws of the RAND study, which CMS uses to defend its position that physicians are not seeing patients for follow-up care, we urged CMS to follow the established process of identifying individual codes as potentially misvalued if there is concern with the post-operative visits assigned to a particular service. A blanket approach to address all 010-day and 090-day global surgical packages inappropriately impacts physicians performing surgeries.
Quality Payment Program
In response to several CMS proposed changes to the Quality Payment Program (QPP) Merit-Based Incentive Payment System (MIPS) benchmark and reporting requirements, we raised our continued concerns about increased reporting requirements and how they conflict with CMS’ goals of reducing administrative burden within the MIPS program. Annual program changes increase the administrative burden and complexity of the MIPS program and divert physician time and resources from providing patient care. Physicians who comply with MIPS reporting requirements should be offered a bonus potential for having increased reporting requirements as an incentive to do that work instead of being penalized. We urged CMS to hold harmless all eligible clinicians and groups from a MIPS penalty during the 2023 performance year due to the ongoing circumstances of the COVID-19 pandemic. These flexibilities should be continued until COVID cases are markedly reduced.
SVS responded to CMS’ request for information (RFI) on the potential development of a quality measure which would assess the percent of patients with diabetes who receive neurologic and vascular assessment of their lower extremities to determine ulcer risk and if they receive a follow-up plan of care. We expressed general support for a new measure related to diabetes control that includes a neurologic and vascular assessment and suggested that including a referral to a specialist would enhance the measure’s effectiveness in reducing diabetes-related lower-extremity amputation. However, we noted such a measure would not be appropriate for specialists who are seeing patients after an ulcer has been identified. This measure would be appropriate for primary care providers at the group level within the same specialty and those treating the patients’ underlying conditions who have frequent contact with the patients.
OPPS rule comment letter
We appreciate that CMS has acknowledged the impact of the recent Supreme Court decision on American Hospital Association v. Becerra, which requires CMS to apply a rate of ASP (average sales price) +6% to drugs and biologicals. We urged CMS to provide as much detail as possible in the final rule related to the conversion factor modifications that will impact HOPPS payments as a result of the revised 340B drug payment policy and provide opportunities for public input regarding how it will conduct retrospective policy changes if such changes are necessary.
In CMS’ comprehensive Ambulatory Payment Classification (APC) methodology, if two J1 services are reported together and meet specific frequency and cost criteria, a complexity adjustment can be applied, thus moving the payment rate to the next highest APC. We requested that CMS allow a complexity adjustment for CPT Code pair 37187 (venous thrombectomy) and 37248 (venous balloon angioplasty) based on frequency and cost data. CMS currently recognizes CPT Code pair 37187 (venous thrombectomy) with 37238 (venous stent) for complexity adjustment consideration.
In the 2020 OPPS/ASC (ambulatory surgical center) final rule, CMS established a prior authorization process for certain hospital outpatient department (HOPD) services, which is now being applied to vein ablation. We are concerned that CMS continues to misinterpret an increase in the volume of utilization for certain procedures in the HOPD setting as “unnecessary,” when such increases may reflect an appropriate site-of-service shift, a change in practice guidelines, decreases in corresponding/related services or changes in coverage determinations.
We urged CMS to holistically review data (i.e., site of service, guidelines, coverage determinations, etc.) prior to expanding prior authorization requirements.
Temporarily office-based
CMS reviewed CY 2021 volume and utilization data for several procedures, including two vascular duplex scan procedures (CPT Codes 93985 and 93986).
Based on low volume, CMS is proposing to continue to designate these two vascular duplex scan procedures as temporarily office-based for CY 2023. We expressed appreciation for CMS’ proposal to extend the temporary designation for CY2023 to allow for further analysis before determining if it is appropriate to permanently designate them as office-based.
Additionally, SVS opposes CMS’ proposal to change the terminology currently applied to “skin substitutes” to “wound care management products” and encouraged CMS to work with specialty societies and the American Medical Association Current Procedural Terminology (CPT) Editorial Panel to address terminology confusion.
CMS will review the SVS comment letters along with those submitted by other stakeholders and members of the public and will issue final CY 2023 rules for both the MPFS and the OPPS later this fall.
Information on the finalized rules will be provided in SVS publications and resources will be available to assist SVS members in understanding and preparing for the implementation of the new Medicare MPFS and OPPS payment policies in the new year.
Read the full letters at vascular.org/FeeSchedule23Comment and vascular.org/HOPPS23Comment.
Trisha Crishock, Megan Marcinko and Jill Rathbun are members of the SVS Washington, D.C., office.












